Sleep is an essential part of our routine, yet between 50 and 70 million adults in the United States suffer from a sleep disorder, and sleep doesn’t come quickly. Disturbance with sleep can influence us on so many levels—from how low our energy is to productivity and overall mental health. This post will discuss some of the most prevalent sleep disorders, their causes, their signs and symptoms, and their treatments.
What is a Sleep Disorder, and How Does it Impact Your Health?
Sleep disorders are disturbances in sleep quality, timing, and duration. They can also interrupt sleep in various ways, making it difficult to fall, stay, or feel rested upon waking up. Sleep is vital to regain our body and mind in a state of rest from all the daily routines.
The impact of sleep disorders on health can be significant. A lack of quality sleep can have severe effects on your health, such as:
- Physical health
- Mental health
- Emotional well-being
- Daytime fatigue, difficulty concentrating, irritability, and mood swings
- Risk of obesity, diabetes, and heart disease
In addition to serotonin production, sleep disorders can also affect the mental balance of a person. Poor sleep has also been associated with a higher likelihood of suffering from depression, anxiety, and other mental health issues. Additionally, individuals with sleep disorders may also experience cognitive impairments, such as memory problems and difficulty with decision-making.
What are Some Major Sleep Disorders?
A detailed study published in the National Center for Biotechnology Information by StatPearls elaborates on the primary sleep disorders categorized by the International Classification of Sleep Disorders (ICSD).
The ICSD helps provide a standardized classification and definitions for sleep disorders. Specifically, the third edition of the ICSD (ICSD-3) includes the following categories of sleep disorders:
- Insomnia
- Sleep-disordered breathing
- Central disorders of hypersomnolence
- Circadian rhythm sleep-wake disorders
- Parasomnias
- Sleep-related movement disorders
Although these categories are regularly updated following the mass data.
Insomnia: Insomnia involves persistent difficulty falling asleep, staying asleep, or experiencing non-restorative sleep despite adequate sleep opportunities. It can lead to daytime impairment or distress, affecting mood, concentration, and overall quality of life.
Sleep-Disordered Breathing: This category includes disorders such as obstructive sleep apnea (OSA), where breathing repeatedly stops and starts during sleep due to upper airway obstruction. It results in fragmented sleep, loud snoring, and daytime sleepiness.
Central Disorders of Hypersomnolence: These disorders are characterized by excessive daytime sleepiness despite sufficient nocturnal sleep. Examples include narcolepsy, where individuals experience sudden, uncontrollable episodes of sleep during waking hours.
Circadian Rhythm Sleep-Wake Disorders: These disorders involve disruptions in the body's internal clock, leading to difficulties with sleep timing that do not align with societal norms. Conditions include delayed sleep-wake phase disorder (DSWPD) and shift work disorder.
Parasomnias: Parasomnias are abnormal behaviors or experiences that occur during sleep, often involving partial arousal from sleep. Examples include sleepwalking, night terrors, and REM sleep behavior disorder (RBD), where individuals act out vivid dreams.
Sleep-Related Movement Disorders: These disorders involve abnormal movements or behaviors during sleep that disrupt sleep continuity. Restless legs syndrome (RLS) causes uncomfortable sensations in the legs, often relieved by movement, while periodic limb movement disorder (PLMD) involves repetitive limb movements during sleep.
Types of Sleep Disorders
There are over 80 kinds of sleep disorders that have been coined over the years. Here are some more:
Restless Legs Syndrome (RLS): A neurological disorder characterized by uncomfortable sensations in the legs and an irresistible urge to move them, usually worsened during rest or sleep.
Hypersomnias: Conditions characterized by excessive daytime sleepiness despite sufficient nocturnal sleep. Examples include idiopathic hypersomnia and Kleine-Levin syndrome (periodic hypersomnia).
Sleep-related Neuromuscular Disorders: Conditions that affect the muscles or nerves involved in sleep, such as nocturnal leg cramps and sleep-related movement disorders.
Obstructive Sleep Apnea (OSA): OSA is a common disorder where breathing repeatedly stops and starts during sleep due to a blocked upper airway, often causing loud snoring and daytime sleepiness.
REM Sleep Behavior Disorder (RBD): RBD is a parasomnia where individuals act out vivid dreams during REM sleep due to incomplete muscle paralysis. It can be associated with neurodegenerative disorders and is treated with safety measures and medications like clonazepam.
Delayed Sleep Phase Syndrome (DSPS): DSPS is a circadian rhythm sleep disorder characterized by a persistent inability to fall asleep at a socially acceptable bedtime and difficulty waking up in the morning. Treatment involves behavioral interventions and sometimes melatonin supplements to shift the sleep-wake cycle earlier.
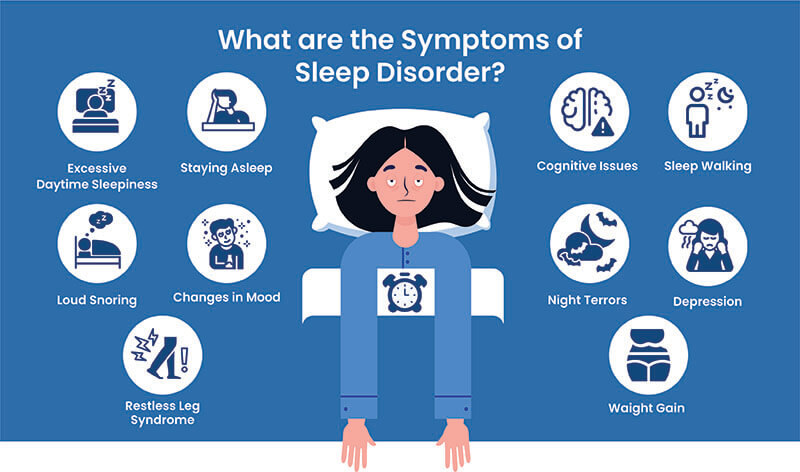
Symptoms of Sleep Disorders
Sleep disorders can significantly impact one's physical, mental, and emotional well-being. Here are some common symptoms of sleep disorders and their potential effects on overall health.
Difficulty Falling or Staying Asleep
One of the primary symptoms of a sleep disorder is difficulty falling or staying asleep. This could manifest in various ways, such as taking a long time to fall asleep, waking up frequently throughout the night, or waking up too early and unable to go back to sleep. The inability to get enough restful sleep can lead to daytime fatigue, irritability, and difficulty concentrating.
Excessive Daytime Sleepiness
Excessive daytime sleepiness is another common symptom of sleep disorders. It refers to feeling excessively tired during the day, even after a full night's sleep. It can cause difficulties in concentrating, working, or completing daily tasks, significantly impacting one's quality of life.
Changes in Mood
Sleep disorders can also affect one's emotional well-being. Lack of sleep can result in irritability, mood swings, increased anxiety, and even depression. These mood changes can further disrupt one's sleep, creating a vicious cycle that can be hard to break.
Loud Snoring
Loud snoring can be a symptom of sleep apnea, a sleep disorder characterized by loud and frequent snoring, gasping for air while sleeping, and pauses in breathing. Sleep apnea can have profound health implications, such as an increased risk of heart disease and stroke.
Restless Leg Syndrome
Restless leg syndrome is a sleep disorder characterized by an uncomfortable sensation in the legs, often described as a tingling, itching, or burning feeling. This sensation can make it challenging to fall asleep and cause disruptive movements during sleep, leading to poor-quality rest.
Mental Health Disorders
Several studies have found a significant link between sleep disorders and mental health disorders such as anxiety, depression, and bipolar disorder. Lack of sleep can exacerbate symptoms of these conditions, making it essential to address any underlying sleep disorders.
Memory and Cognitive Issues
Sleep is vital for consolidating memory and proper brain function. Therefore, those with sleep disorders may experience difficulties in memory and concentration, leading to poor performance at work or school and decreased overall cognitive function.
Weight Gain
Sleep disorders can also affect one's weight. Lack of sleep can disrupt the body's hormones, leading to an increase in appetite and a decrease in metabolism, making it easier to gain weight. It can also impair one's ability to exercise and make healthy food choices, contributing to weight gain.
What Causes Sleep Disorders?
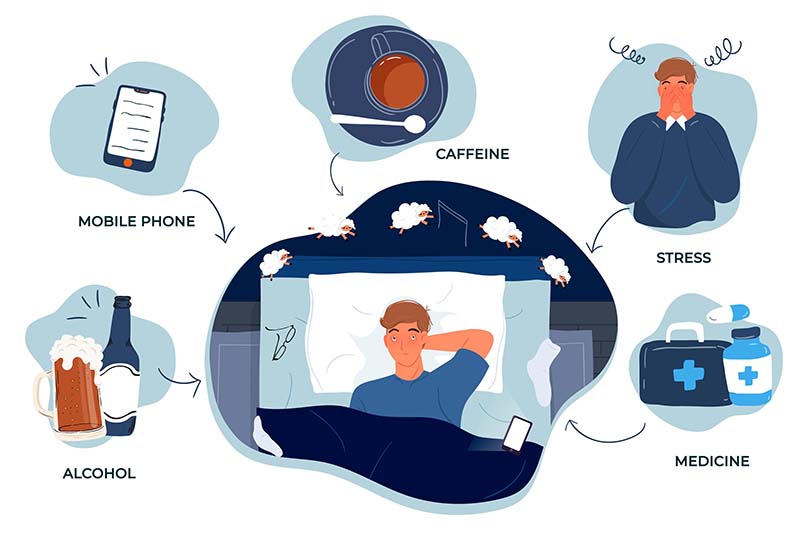
For some people, sleep can be a constant struggle, leading to sleep disorders that can significantly impact their daily lives. In this blog post, we will explore the leading causes of sleep disorders and their potential effects on our health.
Stress and Anxiety: Stress and anxiety release cortisol, disrupting sleep and leading to insomnia, characterized by difficulty falling or staying asleep, and daytime fatigue.
Medical Conditions: Respiratory issues (e.g., asthma, COPD) can cause sleep apnea. Heart disease, diabetes, and chronic pain also disrupt sleep.
Lifestyle Factors: Excessive caffeine consumption, late-night device use, irregular sleep schedules, napping, and poor sleep hygiene affect sleep patterns.
Medications: Some medications (e.g., antidepressants, stimulants, beta-blockers) can cause restlessness, frequent urination, or drowsiness, affecting sleep.
Genetics: Genetic factors contribute to sleep disorders like narcolepsy (excessive daytime sleepiness) and restless legs syndrome.
Environmental Factors: Noise, light, and temperature in the sleep environment impact sleep quality. Noise disturbs falling asleep, and light suppresses melatonin production, affecting staying asleep.
Do Sleeping Positions Affect Sleep Disorders?
Yes, sleeping positions can significantly impact various sleep disorders. For individuals with obstructive sleep apnea (OSA), sleeping on the side is often recommended as it can help reduce airway obstruction, whereas sleeping on the back may exacerbate symptoms.
People with gastroesophageal reflux disease (GERD) may benefit from sleeping on the left side, which can help minimize acid reflux. Side sleeping can also reduce snoring compared to back sleeping, where the tongue may block the airway. For those with restless legs syndrome (RLS), adjusting sleep positions might provide some relief, although effectiveness can vary.
Additionally, individuals with chronic pain may find that side or back sleeping with appropriate support alleviates discomfort, though the best position can depend on the type of pain experienced.
Which Sleep Position is Best for Sleep Disorders?
The best sleep position for managing sleep disorders depends on the specific condition:
- Sleeping on your side (left or right) is often recommended to reduce airway obstruction while sleeping on your back can worsen symptoms.
- Sleeping on the left side is generally advised to reduce acid reflux and improve digestion.
- Side sleeping can help reduce snoring compared to sleeping on your back, where the tongue can block the airway.
- The ideal position can vary; some find relief by adjusting positions or using a pillow to support the legs.
- The best position often depends on the type of pain. For lower back pain, sleeping on the side with a pillow between the knees or on your back with a pillow under the knees can provide relief.
How Can You Diagnose a Sleep Disorder?
Diagnosing a sleep disorder involves:
Clinical Assessment: Gathering medical history, symptoms, and lifestyle factors.
Sleep Diary: Recording sleep patterns over at least two weeks.
Sleep Questionnaires: Screening tools to assess symptoms and severity.
Polysomnography (PSG): Comprehensive sleep study in a laboratory to monitor sleep physiology.
Home Sleep Apnea Testing (HSAT): Portable devices for more straightforward cases of obstructive sleep apnea.
Multiple Sleep Latency Test (MSLT): Evaluates daytime sleepiness, primarily for narcolepsy.
Actigraphy: Wrist-worn device to monitor sleep-wake patterns over time.
Specialized Assessments: Blood tests or consultations with specialists may be required.
How to Treat a Sleep Disorder?
There are various ways you can treat your sleep disorder. Here is a breakdown of different techniques that will help you treat sleep disturbances:
Healthy Sleeping Habits
It is possible to make changes to your sleeping patterns. First, make sure you provide adequate time for your sleep. You could discover that you're happier and more productive during the day if you sleep well every night.
To enhance your sleeping patterns, it might be beneficial to:
- Go to bed in a calm, cool, and dark area. The light from TVs and other electronic gadgets might interfere with your sleep-wake cycle, so avoid doing either.
- Even on the weekends, try to go to bed and wake up around the same time every day.
- Avoid activities that might interfere with your sleep routine, such as working nights or fluctuating schedules. Shift workers or new parents may find this problematic.
- Steer clear of alcohol, nicotine, and caffeine right before bed. While alcohol might help you fall asleep more quickly, it can also make your sleep lighter than usual. Due to this, you are more prone to wake up in the middle of the night.
- Refrain from taking naps, particularly in the afternoon. This may help you sleep through the night.
- Maintain a regular mealtime pattern and stay away from late-night meals.
- Reduce the amount of liquids you consume right before bed. This might help you sleep longer without needing to use the restroom.
- Discover fresh approaches to stress relief. Before going to bed, establish a pattern that helps you de-stress and unwind. Take a hot bath, read a book, or listen to relaxing music. Your healthcare physician can also suggest yoga, meditation, or massage treatment as other relaxation methods.
- Consult your doctor about prescription and over-the-counter medications that could interfere with sleep.
Therapeutic Activities
Therapies for treating sleep disorders can vary depending on the type of sleep disorder and individual needs. Here are some common types of therapies used:
1. Cognitive Behavioral Therapy for Insomnia (CBT-I): CBT-I is considered the gold standard non-pharmacological treatment for insomnia. It focuses on identifying and changing thoughts and behaviors contributing to sleep difficulties. Techniques may include:
- Sleep Restriction: Limiting time spent in bed to match actual sleep time.
- Stimulus Control: Establishing a consistent sleep-wake schedule and associating the bed with sleep.
- Relaxation Techniques: Incorporating progressive muscle relaxation or deep breathing exercises to reduce arousal and promote sleep.
2. Light Therapy: Light therapy, or phototherapy, is used to treat circadian rhythm sleep disorders such as delayed sleep phase syndrome. It involves exposure to bright light, typically in the morning, to reset the body's internal clock and improve sleep-wake patterns.
3. Continuous Positive Airway Pressure (CPAP) Therapy: CPAP is the primary treatment for obstructive sleep apnea. It involves wearing a mask connected to a machine that delivers a continuous flow of air to keep the airway open during sleep, preventing pauses in breathing and improving sleep quality.
4. Orofacial Therapy: Orofacial therapy—a term used to describe exercises for the mouth and face muscles—may treat sleep apnea in adults and children. This treatment improves the muscles that regulate your lips, tongue, upper airway, and face while also assisting in improving the posture of your tongue.

Medications
Medicinal treatments for sleep disorders vary based on the specific condition and individual needs. Here’s a general overview of common sleep disorders and the types of medications that might be used:
1. Insomnia
- Benzodiazepines: Drugs like temazepam and lorazepam can help, but they are generally recommended for short-term use due to risk of dependence.
- Non-Benzodiazepine Hypnotics: Medications such as zolpidem, eszopiclone, and zaleplon are often used for their sleep-inducing effects with a potentially lower risk of dependence.
- Melatonin Receptor Agonists: Ramelteon mimics the action of melatonin and can help regulate sleep-wake cycles.
- Antidepressants: Certain antidepressants like trazodone and doxepin can be prescribed due to their sedative properties.
2. Sleep Apnea
- Continuous Positive Airway Pressure (CPAP): While not a medication, CPAP therapy is the primary treatment for obstructive sleep apnea.
- Medications: In some cases, medications like modafinil may be used to manage excessive daytime sleepiness related to sleep apnea.
3. Narcolepsy
Stimulants: Medications like modafinil and amphetamine-based drugs can help manage excessive daytime sleepiness.
Sodium Oxybate: Used to treat both excessive daytime sleepiness and cataplexy (sudden muscle weakness).
Antidepressants: SSRIs or SNRIs can help manage cataplexy and other symptoms.
4. Restless Legs Syndrome (RLS)
Dopaminergic Agents: Medications such as pramipexole and ropinirole are commonly used to relieve symptoms.
Anti-Seizure Medications: Gabapentin and pregabalin can help reduce the discomfort associated with RLS.
Iron Supplements: If iron deficiency is identified, iron supplements might be recommended.
5. Circadian Rhythm Disorders
Melatonin: Supplements can help adjust the sleep-wake cycle, especially for disorders like shift work disorder or jet lag.
Light Therapy: Although not a medication, exposure to bright light at specific times can help reset the internal clock.
Devices
- Continuous Positive Airway Pressure (CPAP) Therapy: CPAP is the primary treatment for obstructive sleep apnea. It involves wearing a mask connected to a machine that delivers a continuous flow of air to keep the airway open during sleep, preventing pauses in breathing and improving sleep quality.
- Orofacial Appliances: Oral appliances (mandibular advancement devices) treat mild to moderate obstructive sleep apnea or snoring. These devices reposition the jaw and tongue to maintain an open airway during sleep.
Surgical Procedures
- Uvulopalatopharyngoplasty (UPPP): Removes excess throat tissue to widen the airway and reduce obstructions.
- Genioglossus Advancement (GA): Repositions the tongue muscle attachment to prevent airway collapse.
- Hyoid Suspension: Moves the hyoid bone forward to help keep the airway open.
- Inspire Therapy: Uses a surgically implanted device to stimulate the hypoglossal nerve and maintain airway patency.
- Adaptive Servo-Ventilation (ASV): Adjusts airway pressure in real-time to treat central sleep apnea and complex sleep apnea.
- Bilevel Positive Airway Pressure (BiPAP): Provides varying airway pressure levels to assist breathing during sleep.
Final Thoughts
Sleep is essential for overall health, yet many struggle with disorders that disrupt their rest. Identifying and understanding different sleep disorders—like insomnia, sleep apnea, and restless legs syndrome—along with their symptoms, is key to finding effective treatment.
Improving sleep often starts with healthy habits, such as maintaining a consistent sleep schedule and managing stress. For persistent issues, therapies like CBT-I, light therapy, and CPAP can be highly effective. Medications and devices may also help, and in some cases, surgical options might be necessary.
If you have sleep concerns, consult a healthcare provider for a thorough evaluation and personalized treatment plan. Addressing sleep disorders can lead to better health and an improved quality of life.













