Sleep apnea is one of the most common, but least identified commonly known sleep disorders, impacting an estimated 936 million adults around the world and about 30 million people in the United States. Characterized by a repeated cessation of breathing during sleep, sleep apnea can interrupt sleep and increase the risk of heart disease, diabetes, and stroke.
Research shows 80% of moderate to severe cases go unidentified, which is why it is important to be informed. Becoming aware of the main symptoms, primary causes, and simple prevention methods can improve sleep patterns and safeguard long term health.
What is Sleep Apnea?
Apnea while sleeping is a severe disorder classified as a sleep disorder. Associated breathing temporarily stops while sleeping, and resumes for periods from a few seconds to even a minute or longer. This cessation of breathing can occur dozens or hundreds of times throughout the night.
In turn, less oxygen travels through the brain and body, which creates interruptions to the normal sleep cycle while preventing deep, restorative sleep.
There are three types of sleep apnea:
Obstructive Sleep Apnea (OSA): The most common type, which occurs when the muscle's of the throat relax, blocking the airway.
Central Sleep Apnea (CSA): This occurs when the brain doesn't send the proper signals to the muscles that control breathing.
Complex Sleep Apnea Syndrome: This is a condition made up of components of OSA and CSA.
Those who suffer from sleep apnea are likely to snore loudly, gasp for breath during sleep, and be exhausted during the day despite spending sufficient time in bed. In the long term, sleep apnea can lead to substantial health problems including high blood pressure, heart disease, stroke, type 2 diabetes and cognitive decline.
Sleep apnea can affect anyone, but risk factors include obesity, family history, smoking, alcoholism, and older age.
Fortunately, most people can successfully manage sleep apnea, and improve their life quality due to diagnosis & treatment, that include lifestyle changes, CPAP therapy, oral devices, or surgery.
Symptoms of Sleep Apnea
Sleep apnea symptoms differ from person to person, but some of the most common symptoms are:
Loud, continual snoring (usually reported by a bed partner);
Breathing pauses during sleep (reported by someone else);
Gasping or choking episodes during sleep (recorded from the body attempting to restore airflow);
Heavy daytime fatigue or excessive sleepiness regardless of sleeping a full night’s sleep;
Morning headaches, especially due to oxygen deprivation during sleep;
Difficulties with concentration or memory impairment;
Moodiness, irritability, or depression and anxiety;
Waking with a dry mouth or sore throat;
Nocturia - frequent nighttime urination.
Not everyone who snores has sleep apnea. However, if you have persistent symptoms of sleep apnea (especially breathing pauses or extreme daytime sleepiness) you should seek evaluation by a medical professional.
Causes of Sleep Apnea
Sleep apnea occurs when normal breathing is disrupted during sleep. The cause of sleep apnea depends on the type of sleep apnea:
1. Obstructive Sleep Apnea (OSA) - Most common
OSA occurs when the muscles in the throat relax too much during sleep. This, in turn, makes the soft tissues (i.e., tongue, uvula, and soft palate) collapse and block the upper airway. Therefore, airflow is decreased or completely absent.
Risk factors for OSA include:
- Excess body weight (especially around the neck/upper airway)
- Narrow airway (due to genetics, enlarged tonsils/adenoids)
- Older age, which reduces muscle tone in the throat
- Smoking and alcohol use, which further relax airway muscles
2. Central Sleep Apnea (CSA)
CSA is rarer and occurs when the brain cannot send healthy signals to the muscles that help breathing, which leads to a brain-related respiratory issue rather than having an obstructed airway.
Causes may include:
- Stroke or neurological disorders
- Heart failure
- Certain medications (especially opioids)
- High-altitude sleeping
3. Complex Sleep Apnea Syndrome
This can also be referred to as "treatment-emergent sleep apnea" and is a hybrid of OSA and CSA. This can occur in individuals who have been placed on CPAP therapy for OSA and also start developing central apnea events.
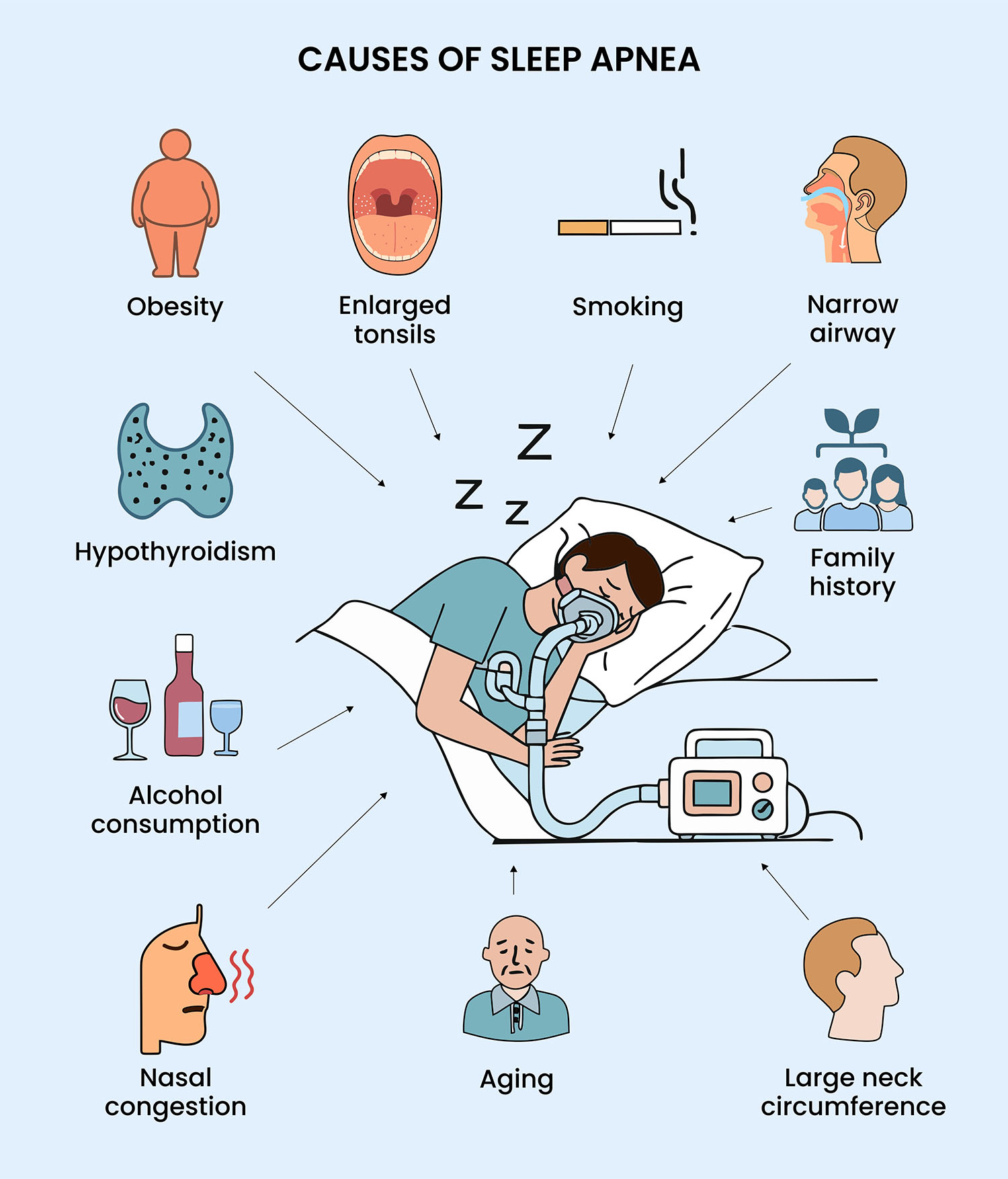
Other Reasons
Obesity & Weight Gain - Excess fat can develop around the neck and chest, narrowing the airway and restricting breathing.
Genetics & Family History - Genetic factors can predispose someone to sleep apnea based on inherited traits, (e.g., naturally narrower throat, oversized tongue, smaller jaw).
Nasal Congestion & Allergies - Obstructed nasal cavities from chronic sinusitis or allergy problems can cause a harder time breathing while sleeping.
Alcohol & Sedatives - Alcohol or sedatives can relax throat muscles too much and will lead to increased airway collapse.
Smoking - Smoking causes congestion and fluid retention; inflammation in the upper airway will increase.
Hormone Conditions - Conditions like hypothyroidism or polycystic ovary syndrome (PCOS) can increase the risk of sleep apnea.
Medical Condition - Conditions like diabetes, high blood pressure, heart disease, and stroke are also linked to sleep apnea.
Age & Gender - Sleep Apnea is more common in men than in women and is more likely as you get older.
Pregnancy - During pregnancy, women experience weight gain and changes in their hormone levels, which can trigger sleep apnea on a temporary basis.
Sleeping Position - Sleeping on your back may fold your tongue and soft palate backwards, shortening the airway.
How to Diagnose Sleep Apnea?
Sleep apnea is frequently unnoticed by the individual, so typically, a possible diagnosis would come down to a medical assessment, which may include overnight testing in order to confirm.
Doctors may utilize their findings, the patient's overall medical history, and any detailed sleep evaluation performed by a specialist to confirm sleep apnea.
1. Medical History & Physical Examination
The doctor will be looking for:
- Loud snoring, pauses in breathing, or gasping (often given by a partner).
- Daytime sleepiness, tiredness/fatigue, lack of concentration.
- Risk factors such as obesity, neck size, alcohol use, or family history.
- Findings in the patient's throat, mouth, and nose, such as enlarged tonsils or obstruction.
2. Sleep Studies (Polysomnography)
An overnight sleep study done at a sleep lab or hospital is the gold standard of diagnosing sleep apnea. The sleep study monitors:
- Brain activity (EEG)
- Eye movements
- Heart rate and rhythm
- Respiration
- Blood oxygen levels
- Muscle activity & snoring
This level of monitoring helps identify the severity of the apnea events.
3. Home Sleep Apnea Test (HSAT) For moderate to severe cases, doctors could suggest a simplified home test. This portable device shows airflow, breathing effort, and blood oxygen levels - all while you sleep at home. While not as thorough as a sleep lab study, a home study is more time-efficient and cost-effective.
4. Specialist Evaluation Depending on results, the doctor may refer you to a sleep specialist, otolaryngologist, or cardiologist to assess for any associated condition and develop the most appropriate treatment options.
Treatment of Sleep Apnea
The treatment of sleep apnea is based on the type of sleep apnea (obstructive, central, or complex) and the severity (mild, moderate, or severe). The underlying principle behind the treatment of sleep apnea is to maintain an open airway during sleep, restore normal breathing patterns, and ultimately, prevent long-term health complications.
1. Lifestyle Changes (First Line for Mild Cases)
- Weight management: Significant weight loss of even 10–15% of body weight may lessen or diminish symptoms in many patients.
- Changing sleep position: Positioning to sleep on the side rather than the back helps to keep the airway open.
- Avoiding alcohol & sedatives: Ingesting alcohol and/or sedatives relaxes the throat muscles, worsening symptoms.
- Quitting smoking: Cigarette smoking creates inflammation and fluid retention in the airway, leading to upper airway obstruction or neglecting therapy.
- Regular exercise: Exercise can improve lung function and help improve sleep.
2. Continuous Positive Airway Pressure (CPAP)
- The most frequently prescribed and effective treatment for moderate to severe obstructive sleep apnea.
- A CPAP (continuous positive airway pressure) machine administers a continuous flow of air through a mask and keeps the airway open.
- Many patients report an immediate improvement in sleep quality and a reduction in daytime sleepiness experienced within the first few uses of the machine.
3. Oral Appliances (Mouthpieces)
- Custom fitted dental devices advance the lower jaw and tongue in order to keep the airway clear.
- Recommended for patients with mild to moderate OSA who are CPAP intolerant.
4. Surgical Treatments (for severe or unresponsive cases)
- UPPP (Uvulopalatopharyngoplasty): It removes tissue from the throat to enlarge the airway.
- Tonsillectomy & Adenoidectomy: most commonly utilized for pediatric OSA.
- Jaw Surgery (Maxillomandibular advancement): The jaw is advanced to increase the size of the airway.
- Implants & Nerve Stimulation (Inspire Therapy): A machine that stimulates the associated muscles of the airway during sleep to maintain an open airway.
5. Treatment for Central Sleep Apnea
- Adaptive Servo-Ventilation (ASV): Changes airflow based on breathing patterns at the time.
- Bilevel Positive Airway Pressure (BiPAP): Applies different pressures for inhaling and exhaling.
- Treat underlying comorbidities: Address heart failure, stroke, or medication side effects that contribute to CSA.
How to Prevent Sleep Apnea?
While considering some cases of sleep apnea cannot be avoided, in particular because of personal genetics or medical conditions, there are many lifestyle changes available to you that would decrease your risk and increase your quality of sleep.
1. Keep a healthy weight
Extra weight, especially in the area of the neck, is more likely to make the airway smaller and increase the chances of blockage. Regular physical activity and a proper diet can help relieve or prevent sleep apnea symptoms.
2. Sleep on your side
When a person sleeps on their back, the tongue and soft palate may fall back into and block off the airway. A side sleeping position can by itself keep the breathing passages open more easily.
3. Limit alcohol and sedatives
Alcohol, sleeping pills, and sedatives prime the throat muscles for relaxation, which all play a role in increasing the likelihood of airway blockages. Reduce or limit any alcohol or sedative use, especially before sleep.
4. Stop smoking
Smoking creates inflammation of the airways and also can cause additional fluid retention behind the airway, which defines and increases airway problems when sleeping.
5. Keep your nasal passages open
If you suffer from allergies or have chronic sinus problems, try using saline sprays, decongestants or any prescribed medications (nasal spray or otherwise) to help limit breathing problems at night.
6. Practice Good Sleep Hygiene
To improve the quality of your sleep, go to sleep and wake up at the same times, keep your bedroom dark and cool, and try to avoid big meals and caffeine before sleep.
7. Treat Underlying Health Conditions
Health issues such as high blood pressure, diabetes, and thyroid disorders can aggravate sleep apnea. Consistent medical treatment will help reduce the likelihood of experiencing more severe symptoms.
When to Consult a Doctor?
Since sleep apnea often develops over time, many individuals misattribute symptoms to simple snoring or being unusually fatigued. However, ignoring the signs may lead to problems. You should seek medical attention if you notice:
- Loud, chronic snoring that keeps your partner awake
- Pauses in breathing, gasping, or choking during sleep (typically noted by someone else).
- Excessive Daytime Sleepiness that interferes with work, driving, or daily life
- Morning headaches, dry mouth, or sore throat on awakening
- Inability to concentrate, memory blips, or altered mood like irritability and depression
- Exacerbated high blood pressure, diabetes, or heart disease company (no other explanation for worsening).
If you experience any of these symptoms, a primary care doctor or sleep specialist to get tested. Most often, the provider will refer to sleep study (polysomnography or home sleep test) to diagnosis you, and will offer any necessary treatment (if any).
Consult as early as possible, and it is better not just for sleep, but to limit risk of serious long-term consequences such as cardiovascular disease and stroke.
Final Thoughts
Sleep apnea is more than just snoring—it’s a serious health condition that affects sleep quality and overall well-being. The good news is, with early diagnosis and proper treatment, it can be managed effectively. Recognizing the symptoms, understanding the causes, and making healthy lifestyle changes are the first steps toward better sleep and long-term health.






















