Chronic Fatigue Syndrome (CFS) affects millions of people worldwide, and yet it is still highly misunderstood as a health condition. The U.S. Centers for Disease Control and Prevention (CDC) estimates between 836,000 and 2.5 million Americans have CFS, but as many as 90% are undiagnosed.
As a long-term, debilitating illness, CFS continues to affect our activities of daily living, often forcing people to cut back hours, or completely withdraw from work or social activities. Understanding or diagnosing CFS is complicated by biological, environmental, and lifestyle factors working together.
Recent studies cry out for early recognition, specific therapy, and supportive cares to reclaim quality of life. In this guide, we examine symptoms, causes and treatment plans that can really help.
What is Chronic Fatigue Syndrome?
Chronic Fatigue Syndrome (CFS)—also referred to as Myalgic Encephalomyelitis (ME)—is a complicated, long-term health condition characterized by extreme, persistent fatigue, which is not improved by rest and debilitating when influenced by physical or mental activity.
The fatigue in CFS is beyond what is experienced as normal tiredness, and can impair day-to-day activities, work duties, and socialization.
A hallmark feature of CFS is post-exertional malaise (PEM), or a major worsening of symptoms following exercise efforts that can be minimal. This "crash" can persist for days, weeks or more and makes pacing and energy conservation key mechanisms for management.
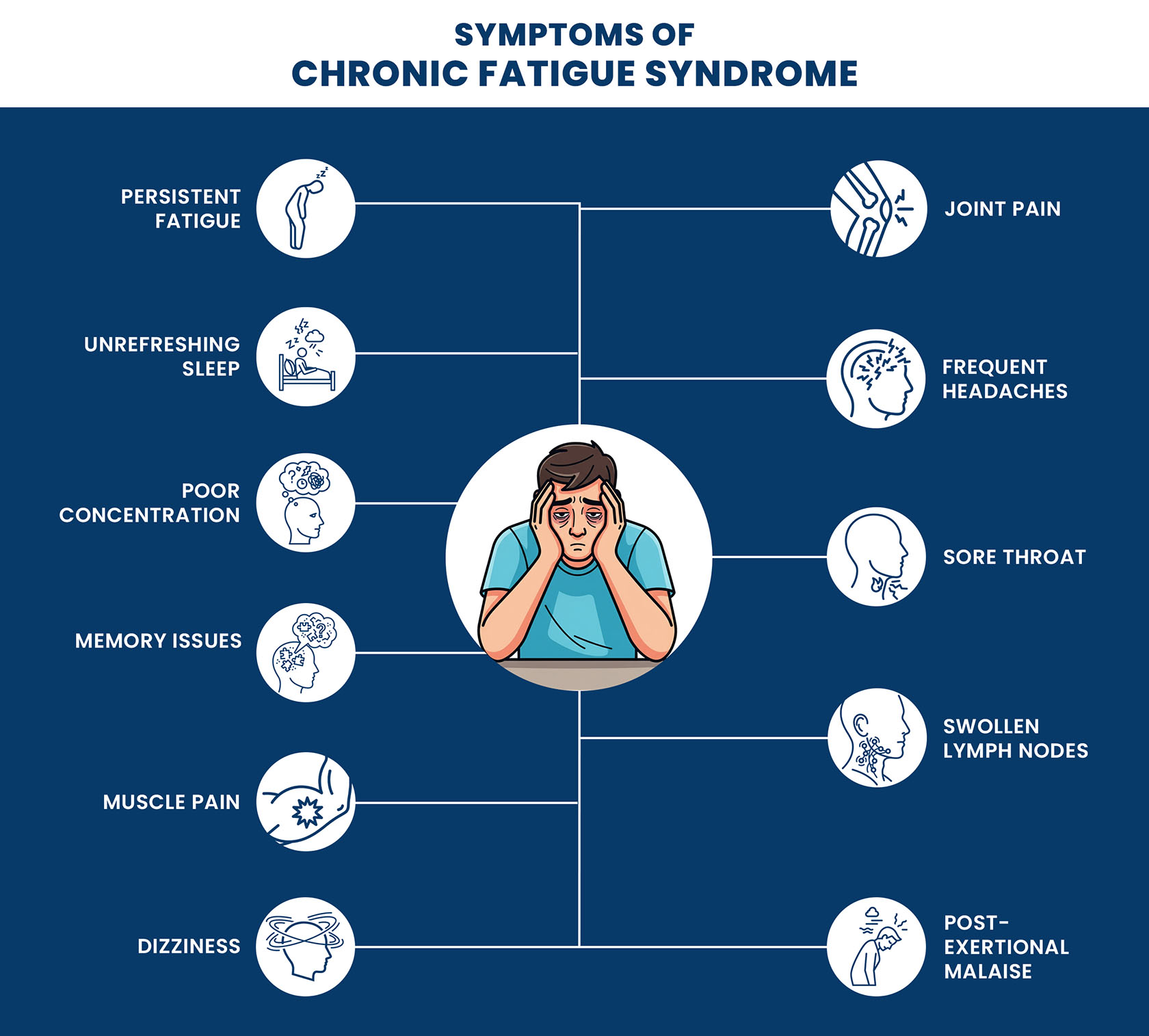
In addition to fatigue, chronic fatigue syndrome symptoms can be varied and vast. These include:
- Unrefreshing sleep
- Cognitive difficulties (“brain fog”) including poor memory, impaired concentration, and slowed processing of information
- Dizziness or lightheadedness—especially when standing (orthostatic intolerance)
- Muscle and joint pain without evidence of inflammation
- Headaches or migraines that are new or worse than before
- Sensitivity to light, sound, or changes in temperature
CFS can affect anyone, but is most common among women aged 40-60. It can emerge suddenly—often following an infection or stressful event—or gradually over time.
CFS is unpredictable and differs in severity. Some individuals can manage daily life with adjustments, while others may experience lengthy periods in which they are housebound or bedridden.
Its impact goes far beyond just physical health. Many people are grappling emotionally and socially, such as exposed to isolation, loss of independence and in some cases an inability to get a diagnosis, since there is no definitive test. Therefore, CFS is often regarded as an "invisible illness," despite having effects which alter lives.
Causes of CFS/Myalgic Encephalomyelitis
The precise cause of chronic fatigue syndrome (CFS) is still unknown - however, research has shown CFS is likely to develop from a mix of biological, environmental and maybe genetic causes that interfere with the body's ability to recover and regulate energy.
Clearly, a single trigger does not explain all cases, but the following factors have been specifically linked to the onset of CFS in several studies:
Viral and bacterial infections – Many cases arise after illnesses, including Epstein–Barr virus, human herpesvirus 6 or some bacterial infections, indicating infections may trigger abnormal immune reactions.
Immune system dysfunction – Individuals with CFS often have minor abnormalities in their immune system, such as chronic or low-grade inflammation, or a highly overactive immune system, which likely perpetuates ongoing symptoms.
Hormonal imbalances – HPA axis abnormalities can alter how the body responds to stress, manage sleep, and regulate energy.
Physical or emotional trauma – CFS can be initiated by major life events, including stressors, surgery, or accidents in individuals predisposed to CFS.
Genetic predisposition – Familial tendencies show an inherited component, wherein CFS susceptibility genes have been proposed.
Mitochondrial dysfunction – Recent studies suggest the possibility of dysfunctional energy production in the cells; this may help explain the characteristic fatigue and post-exertional malaise.
CFS is likely multifactorial, meaning that many of these factors may co-occur in the same patient. Identifying a single cause is difficult; therefore, identifying and managing CFS early is crucial.
Risk Factors of CFS
Although chronic fatigue syndrome can develop in anyone, there are specific factors that may increase the potential to develop the illness:
- Age – It is most often diagnosed in people aged 40–60 years.
- Gender – Women are between 2 and 4 times more likely to develop CFS than men.
- Genetics – A family history of CFS and/or similar conditions may indicate some genetic inclination.
- Pre-existing health conditions – If an individual is diagnosed with autoimmune diseases, allergies, or hormonal problems may also increase the risk of CFS.
- Viral or bacterial infections – Individuals with a past history of recurring or very severe illnesses can trigger the illness to develop.
- High stress levels – Chronic stress, both physical and emotional, can impact the immune system, which increases risk.
- Poor sleep patterns – A history of sleep disturbances that seem to be long-term may be involved in the initiation and/or severity of CFS.
The risk factors identified above do not indicate that CFS will develop, but rather demonstrate higher susceptibility to developing CFS for some populations, particularly when an environmental trigger or lifestyle change co-occurs.
How is CFS Diagnosed?
Diagnosing chronic fatigue syndrome (CFS), or Myalgic Encephalomyelitis (ME), can be difficult because there is no singular definitive test for CFS.
Diagnosis relies on the review of symptoms, medical history, and ruling out other possible explanations for fatigue. The physician will typically seek the following:
Comprehensive Medical History – A review of the patient's health history, lifestyle, and progression of symptoms.
Physical Examination – An evaluation of signs that may indicate other underlying illnesses, or related health conditions.
Symptom Assessment – An evaluation of the severity, duration, and pattern of symptoms; especially persistent fatigue longer than six months, unrefreshing sleep, trouble thinking, and post-exertional malaise.
Diagnostic Criteria – The use of guidelines consistent with those from the CDC or Institute of Medicine that require the presence of the core symptoms.
Exclusion of Other Conditions – Utilizing blood tests, imaging, or other assessments, in order to rule out disorders such as thyroid disease, anemia, sleep disorders, or depression.
Specialist Referrals – Referral to neurologists, rheumatologists, or infectious disease specialists when warranted for full evaluation.
Making an accurate diagnosis is critical in order to avoid inappropriate management and provide accurately prescribed treatments and lifestyle recommendations.
Treatment of Chronic Fatigue Syndrome
Chronic Fatigue Syndrome (CFS) treatment addresses symptoms (managing exacerbation), enhanced quality of life, and underlying triggers (if any) and there is currently no cure. A tailored, integrated approach is sometimes best.
Common chronic fatigue syndrome treatments include:
1. Activity Management (Pacing) – Finding the right balance in activity to manage the symptoms, especially after exertion, and to avoid exacerbation of symptoms like post-exertional malaise.
2. Cognitive Behavioral Therapy (CBT) – Assisting the patient to manage the emotional and psychological impact of CFS. Learn more about CBT here.
3. Graded Exercise Therapy (GET) – The gradual increase of stamina through low-level physical activity, closely monitored and unique to the individual (exercising with caution and not exceeding individual limits).
4. Sleep Management – Supporting healthy sleep behaviors and addressing sleep disturbances (insomnia, sleep apnea etc.).
5. Pain Management – Using either over-the-counter or prescription pain medications, physical therapy, and gentle stretching to alleviate muscle and joint pain.
6. Medications for Specific Symptoms – Using specific medications to treat such issues as depression, anxiety, or orthostatic intolerance.
7. Nutritional Support – Using a balanced diet and rectifying deficiencies like vitamin D or B12.
8. Stress-Reduction Techniques – Using mindfulness, meditation, or breathing practices to reduce mental and physical stress.
9. Support Groups and Counseling – Using social connections and emotional support to combat feelings of isolation.
An individualized care plan with a CFS knowledgeable medical professional is essential to properly manage CFS long term.
When to Consult with Your Doctor?
If you are feeling fatigued and symptoms last for longer than six months, you should speak with your doctor, especially if you are becoming worse with physical or mental activity and not improving with rest.
Do seek medical advice if: the fatigue is accompanied by memory and concentration issues, feeling dizzy, vague unexplained muscle or joint pain, frequent headaches, or simply feeling unrefreshed by sleep.
Consulting early is important to rule out any other cause, ascertain an accurate diagnosis, and start management interventions to prevent you declining further in terms of quality of life.
Final Thoughts
Overall, chronic fatigue syndrome influences one’s everyday life. Even a simple chore may be daunting. Although there is no immediate remedy for this condition, a proper diagnosis and adjustments in one’s routine along with the implementations of specific treatment programs ensure that the patient copes with the symptoms of the disease and enjoys a decent quality of life.













