Chronic pain impacts over 1.5 billion people worldwide, making it one of the most prevalent health concerns today. In the United States, approximately 1 in 5 adults suffer from chronic pain lasting longer than 12 weeks—even after the initial injury or illness has resolved.
More than a physical experience, chronic pain impedes daily functioning and mental health while decreasing quality of life. This guide will examine common signs and symptoms, current best practices for treatment, and what you can do to prevent chronic pain from taking over your life.
Whether you are personally experiencing chronic pain or supporting someone who is, this article can provide empirical evidence and first-hand experiences to help you along the way.
What is Chronic Pain?
Chronic pain is defined as pain that lasts 12 weeks or longer, continuing after the injury or disease that caused it has healed. Although acute pain is usually indicative of ongoing damage or injury and generally resolves after further treatment, chronic pain can last for months, or, more rarely, years. It can exist with no apparent physical cause.
According to the data provided by the Centers for Disease Control and Prevention (CDC), the national survey conducted in 2021 found that 20.4% of adults in the United States—that is, one in five people—reported chronic pain. Of the adults surveyed, about 7.4% reported high-impact chronic pain which significantly interferes with daily living.
Chronic pain can be continuous, or it can be intermittent, appearing in waves. It can feel like everything from a dull ache to sharp, shooting pain. Chronic pain affects more than just your body; it also affects emotional functioning, mental well-being, sleep, productivity and quality of life.
Common Types of Chronic Pain
Here’s a list of the most common types of chronic pain:
- Lower Back Pain
- Neck Pain
- Headaches and Migraines
- Arthritis Pain
- Fibromyalgia
- Neuropathic Pain
- Cancer Pain
- Temporomandibular Joint (TMJ) Pain
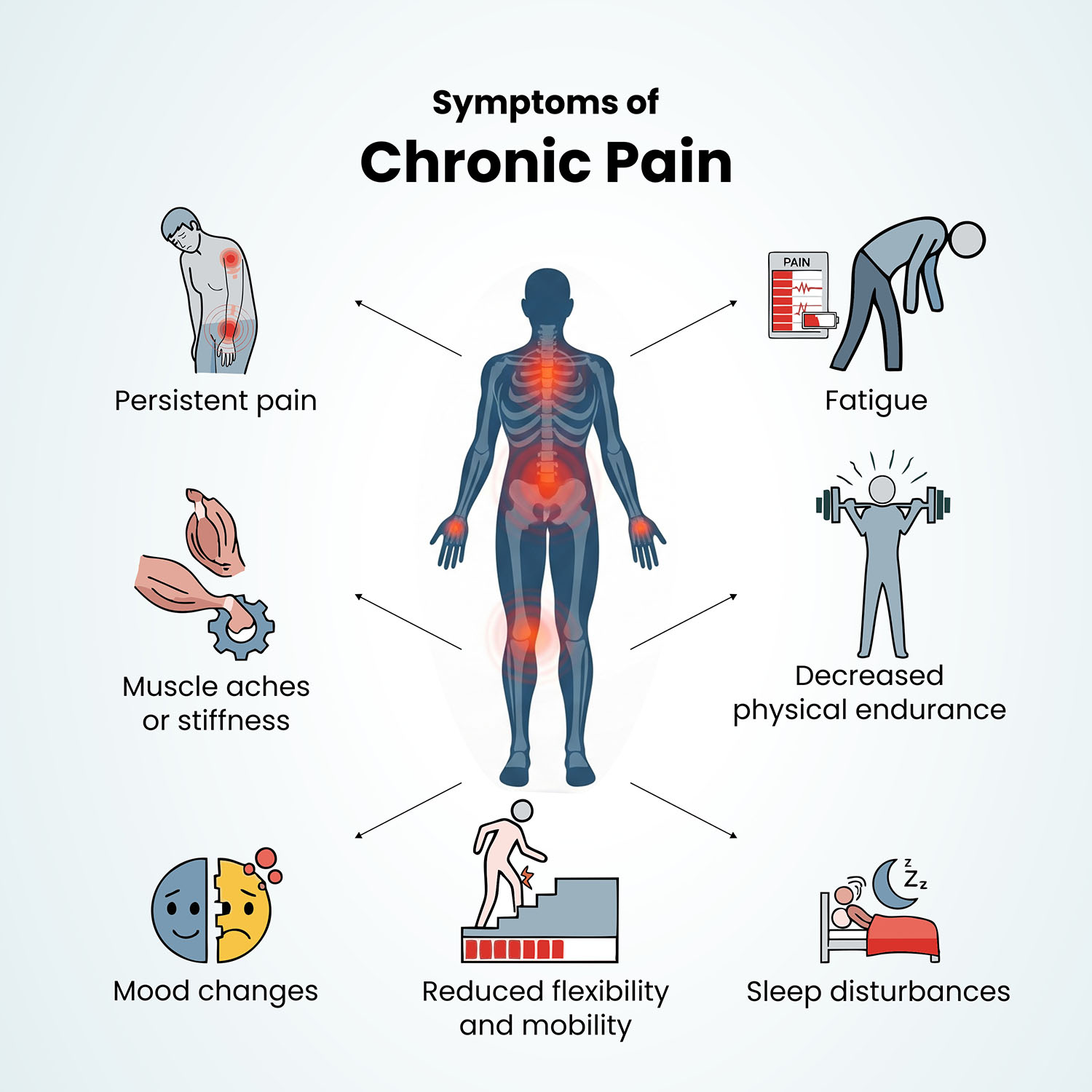
Symptoms of Chronic Pain
Chronic pain is more than just long-lasting discomfort—it often brings a wide range of symptoms that affect both physical and mental well-being. Common symptoms include:
- continuous or recurring pain - dull, sharp, burning, or aching in nature,
- fatigue,
- reduced energy levels, and
- difficulty sleeping due to persistent discomfort.
Mood changes like:
- irritability,
- anxiety, or
- depression,
are frequent, as chronic pain can take a toll on mental health like, major depressive disorder.
Loss of appetite, weight changes, and limited mobility are also common. Over time, chronic pain may affect focus, memory, and the ability to perform daily activities, leading to frustration and a reduced quality of life.
Causes of Chronic Pain
Chronic pain is not a disease in and of itself, but a complex condition that can originate from multiple physical, neurological, or even psychosocial sources. The following are the primary sources of long-term pain:
1. Neuropathic Pain
This type of pain occurs from tissue injury or damage or dysfunction in the nervous system - either in the peripheral nerves or in the spinal cord and brain.
It is often described by patients as burning, shooting, or tingling that may be present even when there is no visible injury.
Common causes include:
- Diabetes (diabetic neuropathy),
- Shingles (postherpetic neuralgia),
- Multiple sclerosis,
- Compression of nerves.
2. Musculoskeletal Pain
This type of pain involves either a problem with the muscles, bones, ligaments, tendons, and joints. Occurrence is usually due to the wear and tear of a lifetime, repetitive strain, trauma, or even poor posture.
Arthritis, myofascial pain syndrome, back pain are among a few. The pain might be aching or throbbing, either way it may get worse with movement.
3. Visceral Pain
Visceral pain has its origins in internal organs such as the stomach, intestines, bladder, and/or uterus. The pain is usually described as deep, squeezing, or cramping, and not always easy to locate. Chronic pelvic pain, irritable bowel syndrome (IBS), and endometriosis are a few examples of visceral pain.
4. Inflammatory Pain
Inflammatory pain is a type of pain caused by inflammation of body tissue due to the immune system calling in code pink! Inflammatory pain is common in autoimmune diseases when the functioning immune system attacks healthy tissue.
CNA examples include rheumatoid arthritis, inflammatory bowel disease (IBD), and lupus. Inflammatory pain is often accompanied by redness, swelling, and warmth.
5. Central Sensitization
There is also complex pain, where the central nervous system becomes so sensitized to pain signals that normal touch and pressure can hurt. People can have widespread pain, fatigue, and cognitive issues.
This phenomenon is a significant characteristic of fibromyalgia and chronic fatigue syndrome. In general terms, complex pain is not always associated with visual damage or inflammation.
Risk Factors of Chronic Pain
Chronic pain doesn't always have a specific identifiable cause as it is often a combination of biological, psychological, and lifestyle risk factors. Some people are at greater risk for chronic pain because of the following risk factors:
1. Age: Older adults are at greater risk due to natural age-related changes such as wear and tear to joints, bones, and muscles. Age-related conditions such as osteoarthritis, spinal degeneration, and neuropathy are common triggers for pain.
2. Injury or Surgery History: Previous injuries can lead to ongoing pain whether they are from accidents, sports, or surgery. In some cases, the nerves that are injured, can lead to pain long after the injury has taken place.
3. Sedentary Lifestyle: Lack of activity can weaken muscles and joints, decrease flexibility and increase your chances of pain. Lack of activity can also cause completely independent issues, as evidenced by an increase in back pain or stiffness in joints when someone is inactive.
4. Obesity: Excess weight adds strain to both the spine, joints, and muscles (especially the knees and hips), as well as the inflammatory process of pain-associated conditions like arthritis.
5. Chronic Illness or Medical Conditions: Chronic pain is associated with conditions like diabetes, fibromyalgia, rheumatoid arthritis, multiple sclerosis, and even cancer. Long duration of inflammation, or nerve damage and injury affects the persistence of pain even further.
6. Mental Health Disorders: Anxiety, depression, and post-traumatic stress disorder (PTSD) will magnify the sensation of pain. They will change how pain is managed, and most often make it more difficult to manage pain.
7. Smoking: Nicotine restricts blood flow where healing occurs, contributing to the worsening of musculoskeletal pain. Smokers are also more likely to report chronic pain in the back and neck.
8. Poor Sleep Quality: Sleep deprivation increases sensitivity to pain and limits ability to recover from pain. Many chronic pain individuals are caught in a cycle of pain and disturbed sleep.
9. Stress: Stress can cause muscle tension and inflammation that cause or exacerbate pain. Stress-rich situations can lead to increased central sensitization in the nervous system, or a heightened responsiveness to stimuli.
10. Genetic Predisposition: Some people may be born with a heightened sensitivity to pain or even conditions like migraines and fibromyalgia, which gives them a family history of risk.
How to Diagnose Chronic Pain?
Chronic pain is typically identified as pain that occurs for longer than 3 months or comes and goes over time. As pain often means something is wrong inside your body, the goal of health professionals is to find the cause of your pain; however, it is not always clear what the pain is related to.
Chronic pain can be difficult to diagnose because it is subjective in nature; only the person experiencing the pain can tell you how it actually feels.
If you are experiencing continuous pain, you should speak to a healthcare provider at that time of an assessment you may be asked:
- Where you have pain?
- How bad it is (normally expressed numerically as a scale from 0-10)?
- How often it occurs?
- How it impacts your work or home functioning?
- What makes it worse or better?
- If you are under stress, anxiety, or emotional pain.
- If you have any previous injuries, surgeries or current medical conditions.
To learn more, your health care provider may perform a physical exam and order a variety of tests, such as:
- A blood or urine tests to check for inflammation and/or infection.
- Imaging scans (X-rays, CT, or MRI) to identify damage in your bones and/or tissues.
- How often it occurs?
- An EMG (electromyography) to determine how your muscles respond to signals.
- Nerve conduction tests to see how well your nerves are functioning.
- Neurological tests to check for reflexes, balance, and coordination.
- An analysis of your spinal fluid (when indicated) may provide you with more details.
All of these tests and examinations help to further define what may be causing your pain, and how to proceed with effective treatment or management.
Chronic Pain Treatment
Managing chronic pain usually involves a complicated plan that is tailored to the person’s condition, symptoms, and treatment response.
The goal of treatment for chronic pain is often to reduce pain, improve function, and enhance quality of life rather than eliminate the pain altogether. Chronic pain can linger even after the initial cause is treated.
Common treatments are:
- Over-the-Counter medications, including non-steroidal anti-inflammatories (NSAIDs) or acetaminophen to relieve mild to moderate pain.
- Prescription medications, including antidepressants, and anticonvulsants, or opioids as needed.
- Topical treatments, including creams or "patches" for localized relief.
- Physical therapy to increase strength, mobility, and pain tolerance.
- Cognitive Behavioral Therapy (CBT) helps with the emotional effects of chronic pain.
- Using mindfulness techniques, such as mindfulness meditation or deep breathing, to reduce stress levels and pain sensitivity.
- Injections such as nerve blocks or steroid injections for inflammation and nerve pain.
- Advanced treatments, such as radio frequency ablation, or spinal cord stimulation, may be suggested.
- Adopting a regular exercise schedule that includes even light activity will help with pain control and improve function.
- Eating a healthy diet, getting enough sleep, and not smoking contribute to managing pain.
- Acupuncture, chiropractic care, and yoga are other forms of complementary treatment for chronic pain relief.
- Biofeedback therapy teaches control over pain-related physiological responses.
- Multidisciplinary pain clinics offer a team-based, personalized treatment approach.
How to Prevent Chronic Pain?
Following are some effective tips to keep chronic pain in check:
- Practice good posture in all of your activities to avoid stressing the joints, back, neck, etc.
- Engage in regular exercise to strengthen muscles, increase flexibility and maintain health of joints.
- Use ergonomic furniture and equipment at work and home to reduce physical stress.
- Avoid repetitive movements or the overuse of certain muscles or joints, without breaks.
- Practice proper lifting techniques when lifting heavy objects, using your legs and not lifting with your back.
- Manage stress using meditation, yoga, breathing techniques etc.
- Get sufficient sleep to allow for the body to heal and repair.
- Eat a balanced anti-inflammatory diet, high in fruits, vegetables and omega 3's.
- Maintain a healthy body weight to reduce stress on the joints and to avoid musculoskeletal pain.
- Manage acute injuries properly so that they do not develop into chronic issues.
- Drink sufficient water to keep your joints and other tissues healthy.
- Avoid smoking as this can restrict blood supply, causing slower healing processes.
- Adhere to your doctor's wishes if you have a condition that could lead to chronic pain (arthritis, diabetes etc.).
When to Consult with Your Doctor?
If you have long-term pain that lasts longer than three months or keeps coming back, even if it is mild, see your doctor. Chronic pain is not just pain that sticks around. It may affect your ability to sleep, your mood, ability to work, or enjoy daily activities.
If pain has diminished your quality of life, causes physical issues with moving around, or you have experienced distress, anxiety or depression because of the pain, you need to see a doctor.
If over-the-counter medicines or home remedies do not help your pain, and your pain seems to get worse over time, do not ignore having a professional assessment.
Final Thoughts
Chronic pain is a multifaceted condition that affects millions of people around the world, not only physically but also emotionally and mentally. Its causes and associated symptoms may differ, however it remains a fact that chronic pain can alter daily life routines significantly.
Recognizing the signs, seeking an appropriate diagnosis and developing a treatment plan, in conjunction with active participation or compliance, has proven to be effective in alleviating and managing pain. In conjunction with this, being preventative and practicing healthy habits, along with early intervention, are also very beneficial.






















