Mental health disorders are a major global concern, with the World Health Organization declaring over 970 million people as having a mental illness worldwide. There are several treatments available to treat mental health disorders. Of those treatments, Cognitive Behavioral Therapy (CBT) is one of the most researched and effective treatments for disorders such as anxiety, depression, PTSD, and OCD.
With a consistent increase in mental health diagnoses, more frequently after the pandemic, understanding when and why you might need CBT can shift your life. This blog covers the fundamentals, the elements of CBT, when it might be recommended, and why CBT gets such support in many mental health systems.
What is Cognitive Behavioral Therapy (CBT)?
Cognitive Behavioral Therapy (CBT) is goal-oriented therapy that helps clients identify negative thought patterns and behaviors. Thinking, feeling, and acting are interrelated and CBT examines cognitive distortions that aren't helpful, then helps clients replace these thoughts with healthier and more constructive thoughts.
CBT can be applied to any mental health diagnosis including anxiety disorders, depression, PTSD, eating disorders, and insomnia. However, CBT is typically not long-term and is problem-focused, which means both clients and clinicians expect there to be homework and practice of thinking changes.
CBT has been shown in many studies to be very effective, and many times clients significantly improve their symptoms after only 5–20 sessions. Core principles of CBT:
- Thoughts, emotions, and behaviors are interconnected
- Negative thinking leads to negative emotional and behavioral responses
- Changing unhelpful thoughts can change emotions and behaviors
- CBT is structured, time-limited, and goal-oriented
- Focuses on present issues rather than experiences
- Emphasizes skill-building and self-help strategies
- Uses collaboration between therapist and patient
- Encourages homework and real-world application
What Conditions Cognitive Behavioral Therapy is recommended for?
CBT is recommended as a first-line treatment by the American Psychiatric Association and NICE UK. CBT is effective at reducing symptoms in 60–80% of individuals when it is a part of the treatment plan, especially when used in combination with lifestyle practices or medications.
Other than school-age children, and virtually any anxious adult battling life and stressors, CBT can provide structure and evaluation of results. Conditions CBT is recommended for:
- Depression
- Generalized anxiety disorder (GAD)
- Panic disorder
- Social anxiety disorder
- Post-traumatic stress disorder (PTSD)
- Obsessive-compulsive disorder (OCD)
- Phobias
- Eating disorders (e.g., bulimia, binge-eating)
- Insomnia
- Substance use disorders
- Chronic pain
- Bipolar disorder (as adjunct treatment)
- Attention-deficit/hyperactivity disorder (ADHD)
- Irritable bowel syndrome (IBS)
- Stress management and adjustment disorders
How Does CBT Work?
CBT is an evidence-based treatment that identifies and helps to challenge negative and unhelpful thinking patterns to help replace them with more positive and helpful beliefs and behaviors.
CBT follows the idea that thoughts, feelings and behaviors are interconnected. When thinking is distorted or unhelpful, it can impact emotional reactions and therefore behaviors as well.
In therapy, you will work with a trained CBT therapist to:
- Explore unhelpful thinking patterns
- Understand how thinking patterns impact your emotions and behavior
- Change patterns of thinking using a more balanced and realistic approach
- Learn behavioral approaches including: exposure, relaxation techniques, setting and achieving goals,
- Developing problem-solving and coping skills for your everyday life
CBT can be structured, goal focused, and also short-term intervention, which makes it a very useful and adaptable approach to a broad range of mental health issues.
How do I get Cognitive Behavioral Therapy near me?
To find cognitive behavioral therapy (CBT) in your area, start with licensed mental health professionals who offer CBT. Many hospitals, clinics, and wellness centers have a mental health department that offers these services. You can also seek recommendations from your primary care provider.
Community health centers and clinics that are affiliated with universities may include CBT in their services at lower price points. Many therapists also offer virtual CBT, which can allow you to complete your therapy without leaving your own home. Be sure to check the education and experience of your therapist for CBT before starting treatment.
Benefits of Cognitive Behavioral Therapy
Cognitive behavioral therapy offers a structured, goal-oriented approach to improving mental well-being. Here's a list of the benefits of cognitive behavioral therapy (CBT):
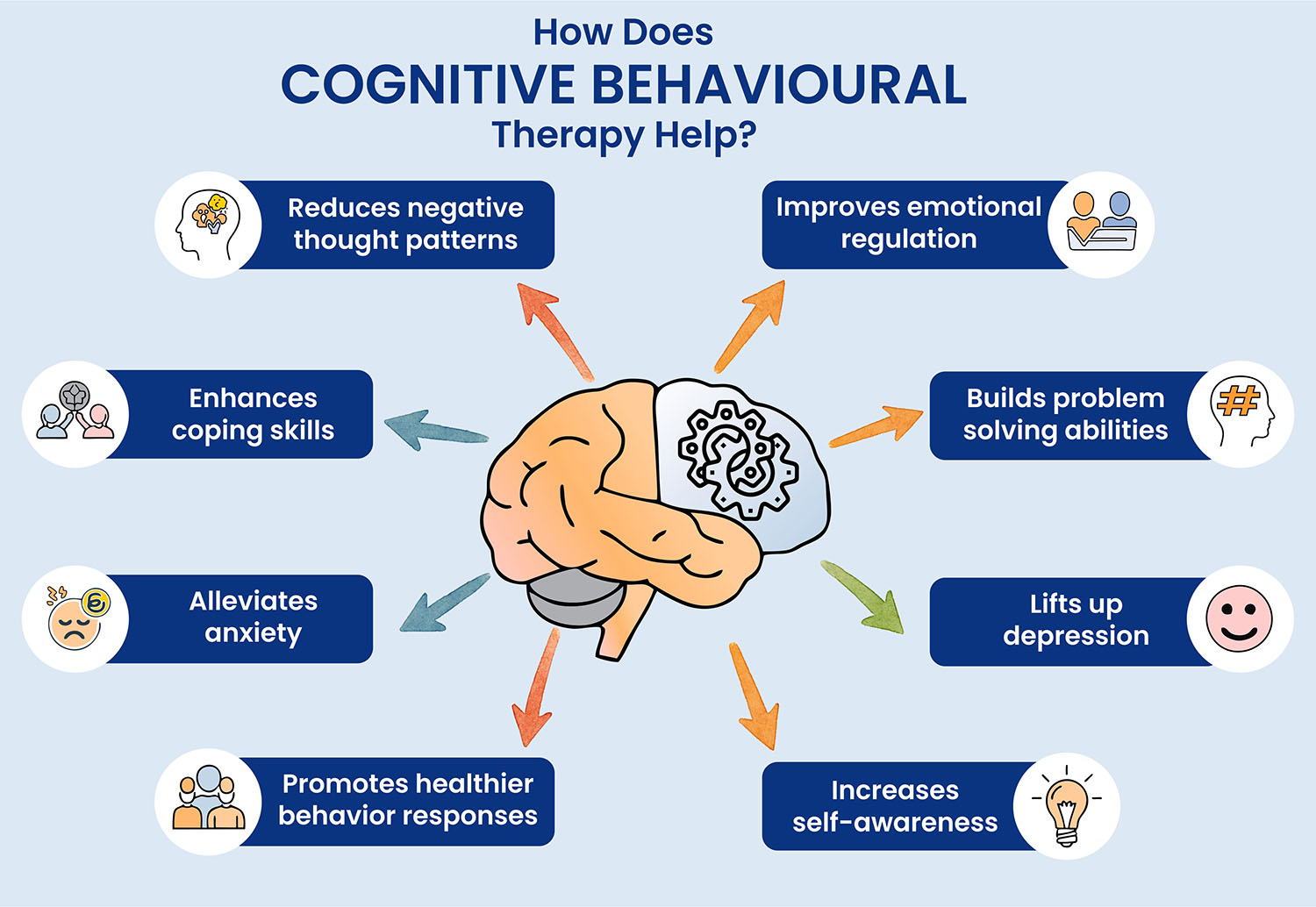
1. Emotional Regulation Improvement: CBT helps you pinpoint feelings that interfere with your life and improve your capacity to manage your unhelpful feelings through the re-evaluation of the thoughts that elicit these feelings.
2. Negative Thought Patterns Change: CBT trains you to notice unbalanced or distorted thoughts and to replace them with more negative or balanced thoughts.
3. Coping Strategies Weakness: CBT provides you with sufficient tools to handle your stress, anxiety, traumas, and challenges in your life more positively.
4. Behavioral Change Awakening: CBT focuses on thinking patterns, which will ultimately lead to behavioral changes directing your improvement to be long-lasting; it does not only mask the symptoms.
5. Create Self-Awareness: CBT encourages you to become more knowledgeable about the interactions between your thoughts, feelings, and behaviors.
6. Evidenced-Based Effective Method of Treatment: CBT has been proven effective for depression, anxiety, post-traumatic stress disorder, obsessive-compulsive disorder, phobias, eating disorders, and many more diagnoses.
7. Structured and Easily Customized: CBT is structured while allowing for you to be treated based on your particular needs.
8. Complements Other Treatments: CBT combines well with medication and other therapies, which allow for a more holistic treatment of an individual.
9. Self-Confidence and Resilience Building: CBT helps develop self-confidence and resilience by presenting fears and challenges in a guided approach, enabling people to build mental strength and independence.
10. Most Cases Resulting in Fast Changes: Many patients experience significant improvements in their mood within a few weeks of treatment with CBT.
Risks of Cognitive Behavioral Therapy
Most people view cognitive behavioral therapy (CBT) as safe and effective. However, like any type of psychotherapy, there are some risks. These are not medically dangerous, but can lead to temporary emotional discomfort.
1. Emotional Distress: CBT typically requires clients to confront emotions, feelings, memories or fears, that are difficult to access at first, and may temporarily worsen distress or anxiety.
2. Not Always Enough for Difficult Mental Health Problems: CBT may not address the entirety of a person’s issues when faced with mental health challenges such as deep-seated trauma, personality-style issues, or very serious psychiatric conditions.
3. Active (and Participatory) Engagement: CBT requires time, energy, and engagement during and outside of therapy, which may be intimidating to some clients.
4. Progress is Often Slow: CBT is not a fast process. Some clients may feel discouraged if they do not see immediate results.
5. Not Always Available: It can be difficult to find a CBT therapist, especially in rural or under-serviced areas, and without support or referrals.
6. May not work for less structured people: Some people prefer a less structured form of therapy that utilizes emotion rather than CBT's more structured and goal based styles.
7. Over-Simplification: In some cases, CBT's focus on present thoughts and behaviors may neglect important unconscious processes or experiences that likewise deserve consideration.
How long does CBT take?
The length of cognitive behavioral therapy (CBT) can depend on the problem being treated, how severe the symptoms are, and individual progress. Most CBT programs are structured, and time-limited:
Short-term CBT - Usually involves between 5 and 20 sessions, often delivered over a number of weeks.
Mild to moderate problems - Some will need between 6 and 12 sessions
Complex/chronic problems - Can take months, or may be delivered over several months in addition to other treatments.
Progress can happen very quickly, often after the first few sessions, and many people notice a significant drop in their symptoms by the 8th to 12th session.
When to Call the Doctor?
You should consider calling a doctor or mental health professional if emotional or psychological symptoms begin to interfere with your daily life, work, or relationships. This includes persistent feelings of sadness, anxiety, irritability, panic attacks, or trouble sleeping and eating.
If you’ve tried self-help strategies but still feel overwhelmed, emotionally numb, or hopeless, it may be time to seek professional support. It's especially important to reach out if you're having thoughts of self-harm or suicide. Early intervention can make a significant difference in managing symptoms and improving long-term mental health outcomes.
Final Thoughts
Cognitive Behavioral Therapy provides a meaningful, structured, evidence-based way to approach various emotional and behavioral issues. Ultimately, it assists people with identifying harmful thoughts and replacing them with healthier, adaptable thoughts.
To put it plainly, CBT helps give people some say over their mental health and positively impacts their overall well-being. CBT is not appropriate for, nor effective for everyone, nor every condition, but there is substantial evidence indicating that it has positive results in addressing issues such as: anxiety, depression, PTSD, etc.













