Sleep and migraines are more closely related than most people think, creating a vicious cycle that can be challenging to break. Inadequate sleep can cause migraines, and migraines can seriously impair sleep, creating a vicious cycle that impacts everyday functioning, mental health, and physical health. Around 75% of migraineurs claim that sleep deprivation is a major trigger for their migraine attacks, and more than 50% report sleep disturbances, according to the American Migraine Foundation.
This extensive guide will examine the science underlying the relationship between sleep and migraines, along with the most typical sleep-related triggers and useful, research-based management techniques. Knowing how these two factors interact is essential to enhancing your quality of life and sleep, regardless of whether you suffer from nightly insomnia, chronic headaches, or sporadic migraine attacks.
What is a Migraine?
A migraine is a neurological condition characterized by severe, pulsating headaches frequently accompanied by other incapacitating symptoms. In contrast to a normal headache, a migraine is a type of headache that can cause significant disruptions to daily activities and last for hours or days. It is a complicated condition involving changes in the brain and nervous system, and it is more than just headaches.
Migraine Phases
Migraines typically progress through four phases, though not everyone experiences all of them:
Prodrome: Subtle warning signs such as mood changes, food cravings, or fatigue that occur 1–2 days before the migraine.
Aura: Visual or sensory disturbances (flashing lights, blind spots, tingling) that may occur before or during the headache.
Attack: The actual migraine headache phase, lasting from 4 to 72 hours if untreated.
Postdrome: A "migraine hangover" with symptoms like confusion, fatigue, and dull head pain after the headache subsides.
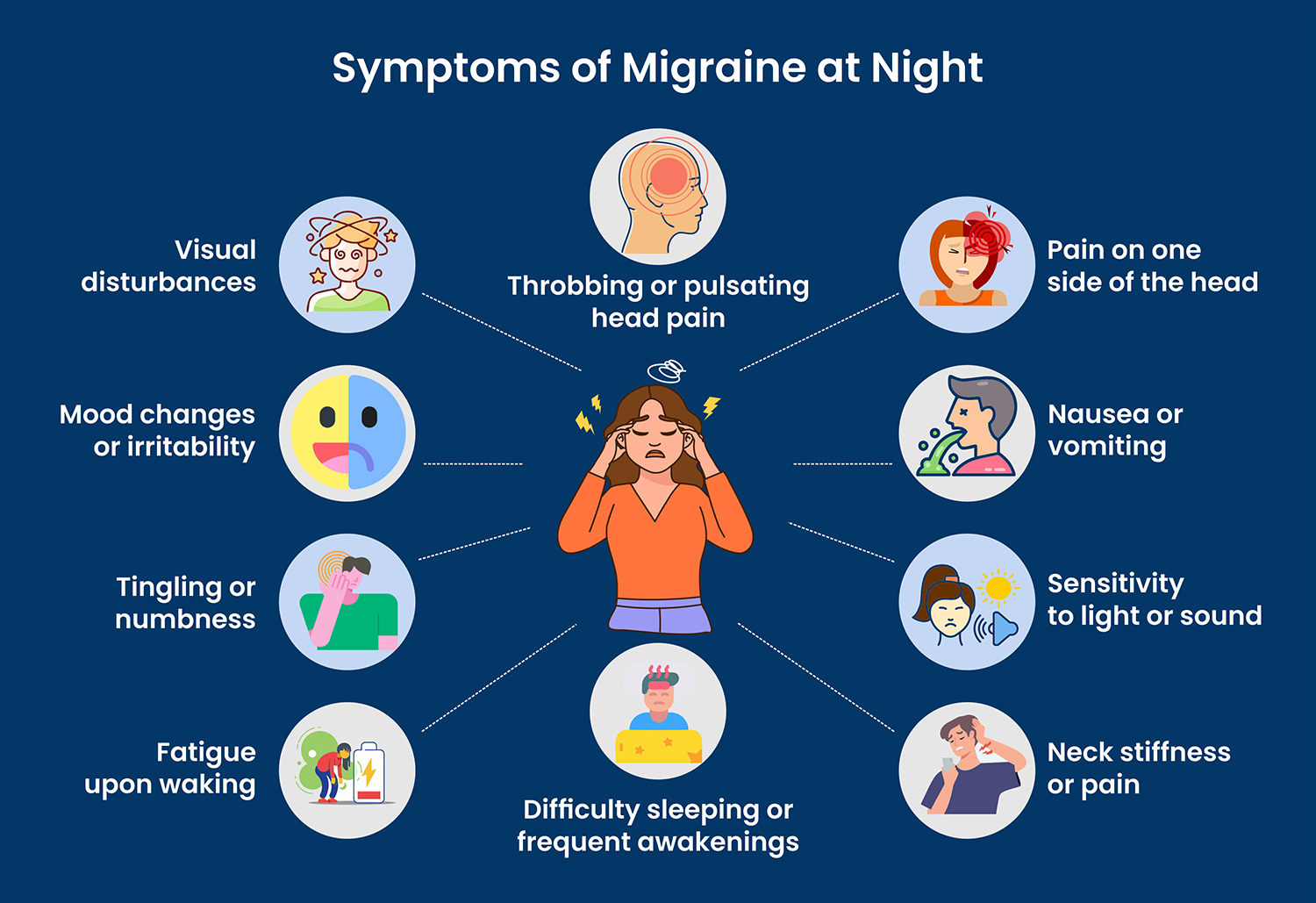
Symptoms of Migraine
Individuals and even attacks can have different migraine symptoms. However, most migraines follow a recognizable pattern and include a combination of physical, neurological, and sensory symptoms. These symptoms can appear in prodrome, aura (optional), attack, and postdrome, though not everyone experiences all phases.
1. Prodrome (Early Warning Signs – Hours or Days Before)
These subtle symptoms may occur 1–2 days before the migraine begins:
- Fatigue or low energy
- Mood changes (irritability, depression, or euphoria)
- Food cravings (often for sweets or salty snacks)
- Stiff neck or muscle tension
- Increased thirst or urination
- Difficulty concentrating
- Frequent yawning
2. Aura (Experienced by About 25–30% of Migraine Sufferers)
Aura usually happens shortly before or during the headache phase and may last 20 to 60 minutes. Symptoms include:
- Visual disturbances (flashing lights, zigzag lines, blind spots)
- Sensory changes (numbness or tingling, usually on one side of the body or face)
- Speech or language difficulties (slurred or confused speech)
- Motor issues (in rare types like hemiplegic migraine, temporary weakness on one side)
3. Attack (Headache Phase)
This is the most intense and recognizable phase, lasting 4 to 72 hours without treatment. Common symptoms:
- Throbbing or pulsating pain, usually on one side of the head
- Moderate to severe pain that worsens with physical activity
- Sensitivity to light (photophobia) and sound (phonophobia)
- Nausea and vomiting
- Blurred vision
- Lightheadedness or dizziness
4. Postdrome (Recovery Phase)
Once the headache subsides, people often experience a "migraine hangover" for up to 24 hours:
- Exhaustion or low energy
- Trouble concentrating
- Mood changes
- Sensitivity to light and sound may linger
- Dull head pain
Less Common Symptoms:
- Nasal congestion or a runny nose
- Abdominal pain or diarrhea (especially in children)
- Cold hands and feet
- Sweating or chills
Why Do You Have Migraine Attacks at Night?
Nighttime migraine attacks, or those that wake you up, can be especially upsetting and may be caused by many underlying factors. Here’s what causes migraines at night:
1. Sleep Disruption or Irregular Sleep Patterns
Inadequate or irregular sleep is one of the most frequent causes of migraines at night. The normal chemical balance of the brain can be upset by fragmented sleep or irregular bedtimes and wake-up times. Insomnia, sleep apnea, and restless legs syndrome are among the conditions that can impair sleep quality and raise the risk of a migraine attack in the middle of the night or early in the morning. A lack of regular sleep can act as a stressor that causes migraines because the brain craves routine.
2. Changes in Brain Chemistry During Sleep
Neurotransmitter levels, including those of dopamine and serotonin, naturally increase and decrease with the stages of sleep. The brain areas in charge of controlling headaches, especially the hypothalamus, and pain pathways, may be impacted by these chemical changes. Any disturbance in the hypothalamus's function while you sleep can exacerbate migraines at night because it also aids in the regulation of sleep-wake cycles.
3. Hypnic Migraines
There is a rare type of migraine called a hypnic migraine, sometimes known as an "alarm clock headache." These migraines are unique because they occur only during sleep and wake the person up, often at the same time each night. While the exact cause is not fully understood, it's believed to be linked to changes in sleep architecture or shifts in brain activity during specific sleep stages. Hypnic migraines typically affect people over the age of 50 and may sometimes respond to low-dose caffeine before bedtime.
4. Accumulated Stress or Tension
A migraine doesn't always happen right away when physical strain, mental tiredness, or emotional stress accumulates throughout the day. Rather, when the body and mind begin to unwind at night, the effects may become apparent. A migraine may start during sleep or right before you try to fall asleep as a result of this delayed reaction. Stress hormone release may disrupt regular brain activity and increase the frequency of headaches at night.
5. Hormonal Fluctuations
The development of migraines is significantly influenced by hormones, particularly in women. During the menstrual cycle, pregnancy, or menopause, levels of estrogen and progesterone may change. Certain times of the day, including the night, may be more susceptible to migraines due to these hormonal changes. Some women experience more frequent nighttime migraines during hormonal changes associated with the use of contraceptives or in the days preceding their period.
6. Dehydration, Skipped Meals, or Caffeine Withdrawal
Your body may react with a migraine hours later, sometimes not until you're asleep, if you didn't get enough water or food during the day, or if you skipped meals. Similar to this, if you're accustomed to caffeine and cut back or avoid it, your body may suffer from withdrawal symptoms, which include migraines. These symptoms typically appear in the early morning when caffeine levels are at their lowest.
7. Medication Timing or Side Effects
Depending on when they are taken, certain medications, particularly those used to treat blood pressure, depression, or sleep disorders, can affect migraine patterns. A migraine may be triggered by a side effect from a nighttime medication dose, or your system may become susceptible to an attack if you skip a dose.
Treatment of Migraine
The two primary types of treatment for migraines are typically acute (abortive) and preventive (prophylactic). While preventive treatment seeks to gradually lessen the frequency, intensity, and duration of migraine attacks, acute treatment seeks to alleviate symptoms during an attack.
1. Acute (Abortive) Treatment
This type of treatment is used to prevent or reduce symptoms such as light or sound sensitivity, headache, and nausea during a migraine attack. The earlier the medication is taken during an attack, the better it usually works.
Typical drugs include:
- Over-the-counter analgesics like acetaminophen, aspirin, or ibuprofen. For mild to moderate migraines, these work best.
- Prescription drugs known as triptans (such as sumatriptan and rizatriptan) target the brain mechanisms responsible for migraines. In addition to relieving related symptoms like nausea, they work well for moderate to severe migraines.
- When trips are not effective or appropriate, older medications called ergotamines, such as dihydroergotamine (DHE), may be used.
- If the migraine is accompanied by nausea or vomiting, anti-nausea drugs (such as prochlorperazine or metoclopramide) may be helpful.
- Newer classes of drugs called ditans (like lasmiditan) and gepants (like rimegepant and ubrogepant) are safer for patients with cardiovascular problems because they treat acute migraine without constricting blood vessels.
2. Preventive (Prophylactic) Treatment
When migraines occur frequently (more than four days per month), are extremely severe, or substantially lower quality of life, this kind of treatment is taken into consideration. Reducing the frequency and severity of migraines is the aim.
Options include:
- Beta-blockers (propranolol), calcium channel blockers, antidepressants (amitriptyline), and anticonvulsants (topiramate or valproate) are examples of prescription drugs that were initially created for other conditions.
- Newer injectable drugs called CGRP inhibitors (such as galcanezumab, fremanezumab, or erenumab) are made especially to stop migraines by preventing the calcitonin gene-related peptide pathway, which is implicated in migraine attacks.
- For chronic migraines, the FDA has approved Botox injections (onabotulinumtoxin A), which are given by a medical practitioner every 12 weeks.
3. Lifestyle Modifications
Lifestyle is a key factor in migraine management for both forms of treatment. A regular sleep schedule, stress management with cognitive behavioral therapy or relaxation techniques, drinking plenty of water, avoiding known food triggers, and regular, moderate exercise are all common recommendations.
4. Non-Pharmacological Therapies
Some people have found success with complementary therapies like biofeedback, acupuncture, physical therapy, and specific supplements (like coenzyme Q10, magnesium, and riboflavin). These techniques are typically used in conjunction with medication and lifestyle modifications rather than in place of them.
5. Neuromodulation Devices
Additionally, there are medical devices that target the nerves involved in migraines using electrical or magnetic stimulation. These consist of vagus nerve stimulation (VNS), transcranial magnetic stimulation (TMS), and external trigeminal nerve stimulation (eTNS). These are particularly helpful for those who have not responded well to medications or who would rather not take them.
How Does Migraine Pillow Help?
A migraine pillow is made especially to support spinal alignment, ease muscle tension, and enhance sleep posture—all of which can help prevent or lessen migraines. Here are some of the best pillows for migraines:
- Cervical Pillows (Orthopedic or Contour Pillows)
- Memory Foam Pillows
- Cooling Gel Pillows
- Water-Based Pillows
- Buckwheat Pillows
- Latex Pillows
- Aromatherapy Pillows
A migraine pillow can help in the following ways:
1. Supports Proper Neck and Spine Alignment
In particular, the cervical spine may be strained by improper neck alignment while you sleep, which can lead to tension-type headaches or migraines. An ergonomically contoured migraine pillow maintains your spine in alignment and supports the natural curve of your neck. This lessens the possibility of nerve compression or muscle tightness during the night, which can cause a migraine when you wake up.
2. Reduces Pressure Points
Memory foam or other flexible materials that fit your head and neck are used in many migraine pillows. This lessens the pressure on delicate spots, particularly those near the base of the skull and upper neck, which are frequently affected by cervicogenic headaches (headaches that originate in the neck). The likelihood of migraine pathways being activated while you sleep can be decreased by lowering pressure in these areas.
3. Minimizes Movement and Enhances Sleep Quality
A well-made pillow lessens tossing and turning at night by keeping your head in a stable position. Deeper, more restful sleep can result from fewer movements. Improving sleep quality can help break the cycle of frequent migraines that occur at night or in the early morning, as poor or fragmented sleep is known to trigger migraines.
4. Helps With Temperature Regulation
Certain migraine pillows have breathable materials or cooling gel layers to help control the temperature of the head and neck. For some migraineurs, particularly those who are sensitive to temperature changes, overheating while they sleep can be a subtle trigger. Staying cool can help you sleep better and experience fewer night sweats.
5. Eases Tension and Promotes Relaxation
Tense neck and shoulder muscles that accumulate tension throughout the day can be eased with a migraine pillow. Those who physically carry stress in their upper body should pay particular attention to this. The pillow may lessen stress-induced muscle tension that can exacerbate migraines by encouraging a more relaxed sleeping position.
Final Thoughts
There is no denying—and frequently understated—the connection between sleep and migraines. Migraines can seriously impair sleep, and poor sleep can cause migraines. This vicious cycle can impact your mood, energy, and day-to-day functioning. A proactive and individualized strategy is needed to break this cycle.
Little changes can make a big difference, from lifestyle modifications and medical treatments to the use of supportive equipment like migraine pillows. Migraines can be less frequent and less severe if proper sleep hygiene is prioritized, stress is controlled, hydration is maintained, and triggers related to posture and the neck are addressed.













