Are you one of those many people who frequently endure terrible headaches and migraines? Have you tried everything, from medicines to diet changes, but were unable find relief? Apart from a few medical reasons, the position you sleep in and the kind of pillow you use can also be one of the primary reasons why you are experiencing migraine headaches.
It may sound unbelievable, but getting a better pillow and switching your position can significantly prevent debilitating headaches and migraines. Let's now discover more about how changing such a seemingly small thing can substantially impact our health and general well-being.
What is a Migraine?
Migraines are a type of headache characterized by intense throbbing pain, usually on one side of the head. It is estimated that around 1 in 7 people globally suffer from migraines, making them a common and debilitating condition.
Migraines are not just a typical headache. They are a neurological condition that affects the brain and its blood vessels. The exact cause of migraines is still unknown, but it is believed that they are triggered by certain factors such as hormonal changes, stress, certain foods, and environmental factors.

The symptoms of migraines can vary from person to person but typically include severe head pain, nausea, sensitivity to light and sound, and sometimes even vomiting. The pain can last anywhere from 4 to 72 hours and can be so severe that it interferes with daily activities and quality of life.
The following are the reasons for migraine:
- Family history
- Fluctuations, especially in women
- Alcohol, caffeine, chocolate, MSG
- High or sudden stress
- Lack of or excessive sleep
- Bright lights, strong odors, weather changes
- Intense or sudden exercise
- Frequent use of headache meds
- Loud noises, strong smells
- High blood pressure, sinus infections
- Skipping meals
- Reducing or stopping caffeine
Difference between Migraine and Headache
Aspect |
Migraine |
Headache |
|---|---|---|
| Pain Type | Often throbbing or pulsating | Can be dull, aching, or pressing |
| Location | Typically unilateral (one side of the head) | Can be unilateral or bilateral (both sides) |
| Duration | Lasts 4 to 72 hours and may have multiple episodes | Usually shorter, from minutes to several hours |
| Associated Symptoms | Nausea, vomiting, sensitivity to light and sound | Generally, less severe symptoms |
| Triggers | Specific triggers like stress, certain foods, hormonal changes | Common triggers include dehydration, tension, or lack of sleep |
| Severity | Moderate to severe; can significantly impair daily activities | Mild to moderate; typically manageable |
| Aura | May consist of visual disturbances, tingling, or speech changes | Not typically associated with an aura |
| Response to Medication | Often requires specific migraine medications or treatments | Common pain relievers like ibuprofen or acetaminophen are usually effective |
| Impact on Daily Life | Can cause significant disruption, impacting daily activities | Often less disruptive, but can still cause discomfort |
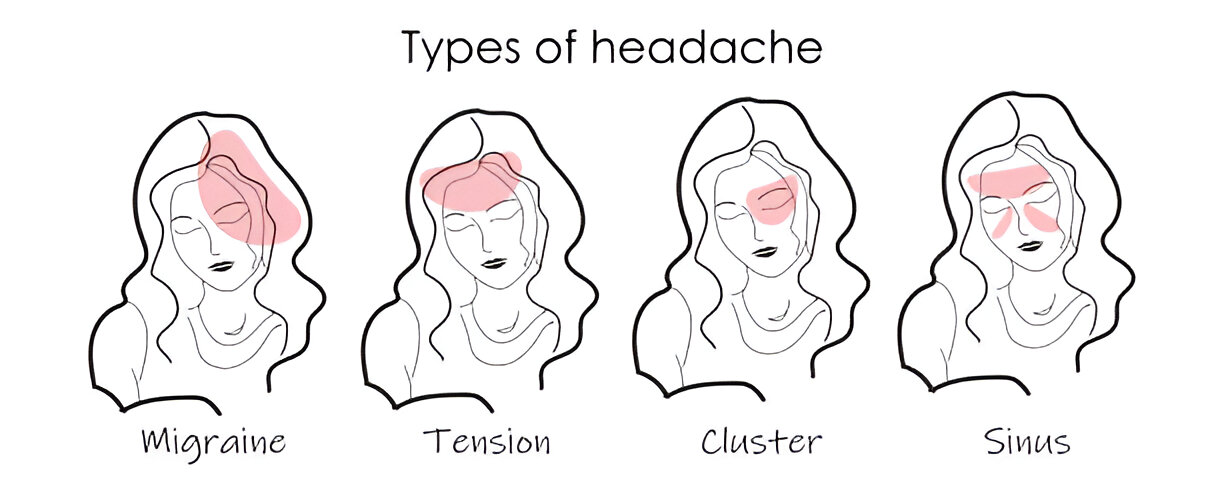
Types of Headache
Headaches can be classified into the following categories:
Tension
Tension headaches are mild to moderate, dull, and steady pain that feels like a tight band around the head. They are often caused by stress, anxiety, poor posture, or muscle tension in the neck and shoulders.
These headaches typically affect both sides of the head and can last 30 minutes to several hours. Over-the-counter pain relievers such as ibuprofen or acetaminophen are effective treatments, as are stress management techniques like relaxation exercises and improving posture.
Migraine
Migraines are severe headaches that can cause throbbing pain, often on one side of the head, nausea, vomiting, and sensitivity to light, sound, or smells. They can last anywhere from a few hours to several days and are typically disabling. Migraines have complex causes, including genetic factors, abnormal brain activity, and changes in neurotransmitter levels like serotonin.
Treatment may involve medications such as triptans or NSAIDs to relieve pain during attacks, preventive medications to reduce frequency, and lifestyle changes to avoid triggers like certain foods, stress, or hormonal changes.
Cluster
Cluster headaches are intensely painful and occur in clusters or cycles, often around one eye or on one side of the head. They are relatively rare, but they are one of the most debilitating headache types. Cluster headaches can occur several times in a day and last from weeks to months, with periods of remission separating them.
Cluster headaches include a variety of associated symptoms, including tearing, redness, and congestion in the affected eye or nostril. Treatment options include oxygen therapy, triptans, and other medications. Preventive treatment, to manage and reduce the frequency of attacks, may be prescribed too.
Sinus
Sinus headaches are caused by inflammation or congestion of the sinuses, often resulting from infection (sinusitis) or allergies. The pain is typically localized in the forehead, cheek area, or around the eyes and may be aggravated by bending forward or sudden movements.
Other symptoms include nasal congestion, pressure in the face, and drainage.
Treatment targets the underlying problem, definitely with antibacterials for bacterial infection; unless there's specific inflammation or swelling present, decongestants or nasal saline sprays are recommended; additionally, nonprescription pain-relievers for symptomatic treatment.
Preventive management of allergies or other contributing factors is important to reduce recurrence of sinus headaches.
How Sleep Position Influences Migraines?
Your sleep position can affect how often you have migraines, and how severe they are. Here’s how:
Pressure on the Neck
If your sleeping position puts pressure on your neck, that could lead to tension headaches. Those tension headaches might then turn into migraines later that night or during the evening. Misalignment during sleep, or position pressure on the neck can occur when sleeping on too high, or too low a pillow.
Spinal Alignment
Good spinal alignment is necessary to reduce headaches. Sleeping positions to encourage good spinal alignment, such as sleeping on your back and using a supportive pillow can reduce strain on the neck and the shoulders. This may reduce the chance of a migraine.
Sleep Apnea
Sleeping in certain positions, especially on your back, can worsen sleep apnea, a condition that interrupts breathing during sleep and is associated with a higher risk for migraines. Sleeping on your side can alleviate some of the issues associated with sleep apnea.
Comfort and Support
Sleeping on an uncomfortable mattress, or an unsupportive pillow can compromise sleep quality and contribute to risk of migraines. Being in a sleep environment that supports your body is important.
Reflux and GERD
If you experience gastroesophageal reflux disease (GERD), it's usually not helpful to sleep flat on your back as this could worsen symptoms. Elevating the head of the bed and/or sleeping on your left side could lessen acid reflux and associated migraines.

How Can You Treat Migraine?
Migraine treatment usually requires a combination of lifestyle changes, medications, and alternative therapies. Below is a list of some options that may alleviate migraine symptoms:
1. Lifestyle Changes
- Continue to maintain a migraine diary to record the potential triggers of your migraine burden; certain foods, stress or other environmental influences, and try to avoid them.
- Staying on a regular sleep schedule, eating regularly and having a generally balanced lifestyle could all help to lessen the occurrence of migraines.
- Some approaches that may help to lessen stress relief, a common trigger.
2. Medications
- Mild migraines can be treated effectively with medications such as ibuprofen, aspirin and acetaminophen.
- In the greater case, the doctor can recommend medications called triptans like sumatriptan or ergotamines.
- In the case of frequent migraines, the patient may be recommended preventive medications such as beta-blockers, antidepressants, or anti-seizure medications.
3. Alternative Therapies
- This practice allows the individual to manage physiological functions such as heart rate and muscle tension, which can decrease episodes of migraines.
- Some people may find relief from frequency of migraines with acupuncture, which involves placing thin needles into specific points on the body.
- Regular massage in and around the neck and shoulders can help decrease muscle tension, which can lead to decreases in migraines.
4. Dietary Changes
- Dehydration can be a trigger, so make sure to drink enough water each day.
- Eating at regular times and making sure to eat balanced meals can help avoid changes in blood sugar that can trigger migraines.
- Be aware of common migraine triggers and minimize your consumption of them. This includes caffeine, alcohol, and some aged cheeses or cured meats.
5. Rest and Sleep
- Try to get consistent, good sleep each night, which can help prevent migraines triggered by disturbances in sleep.
- Make sure that your sleep area is conducive to sleep, with a comfortable mattress and pillow to support alignment.
How Can Your Pillow Contribute to Headache?
If the pillow is not placed in the right position, it may cause poor neck alignment, which can ultimately result in muscle strain and tension that causes headaches.
For example, a pillow that is too low or loop could force your neck to bend at an angle that causes strain because of uneven pressure down the cervical spine and surrounding muscles.
This strain could cause tension headaches or trigger or worsen migraine headaches. A pillow for migraines could lessen that neck strain because its contouring provides the proper support to the head and the spine is in a neutral position.
Also, the pillow’s height and firmness should be catered to your sleeping position—people who sleep on their backs need a medium-firm pillow that will hold the neck in place while not pushing the head too far forward. A side sleeper may need a more firm pillow that will hold the gap between their head and the mattress.
What are the Good Pillows for Migraine and Headache?
- Cervical Pillows: These pillows support the natural curvature of your neck which can keep your alignment ergonomic and alleviate strain.
- Contoured Memory Foam: These pillows provide firm support while conforming to the shape of your head and neck relieving pressure points and offering comfort.
- Cooling Gel: If you are heat sensitive or are experiencing night sweats, these pillows can help regulate temperature and cool you down.
- Adjustable Loft: These pillows also have adjustable height and fill. You can add or remove filling until the firmness and height suits you.
- Buckwheat pillows: These pillows conform to the shape of your head and neck and provide consistent support while allowing air circulation, which can help with heat regulation.
Factors to consider when buying Migraine Pillows
- Pillows that provide the possibility of adjusting the pillow’s height or firmness can help you find the ideal positioning to support spinal alignment, while relieving tension in the neck and shoulders.
- Pillows with cervical support or ergonomic contours can help keep the neck aligned and relieve pressure points, and may help alleviate headaches.
- Memory foam pillows will contour to your head and neck area, providing consistent support and reducing pressure, which can help prevent the unflattering effects of tension headaches.
- Gel-infused memory foam pillows also provide additional cooling properties, which may help if you are heat sensitive and obtain migraines.
- Latex provides firm support and breathability. It will keep your neck aligned and is beneficial if you prefer a more supportive pillow with some bounce.
- A buckwheat pillow will conform to the shape of your head and neck while offering even structure to retain head and neck support, while also permitting airflow and cooling as necessary.
Final Thoughts
It may be surprising to some, but just upgrading to a new pillow can be transformative in treating and preventing headaches and migraines.
Finding a pillow that keeps the spine in proper alignment, reduces tension in the neck, and accommodates the sleeping position helps improve sleep quality and lessen the duration and intensity of migraines.
Regardless of whether you decide on a cervical support pillow, a contoured memory foam pillow, a cooling pillow, or even one with adjustable loft, it is necessary you select one that fulfills your needs in both comfort and support.
Additionally, the firmness of the pillow, the material, whether that be synthetic or natural, and the cooling properties will certainly contribute to better sleep and reduced headaches upon awakening.













