Sleepwalking is a common type of parasomnia that ultimately affects children and adults all around the world. Estimates show that nearly 17% of children and 4% of adults will have at least one instance of sleepwalking in their life.
Instances of sleepwalking vary from harmless wandering to dangerous activities, typically occur in the non-REM stage of deeper sleep.
Sleepwalking usually occurs more commonly between the ages of 4 and 8, while sleepwalking episodes in adults come from underlining triggers largely including stress and sleep deprivation, or medical episodes. Identifying the early warning signs and possible contributing factors is key to managing the sleep disorder and preventing any effects.
What is Sleepwalking?
Sleepwalking, or somnambulism, is a form of parasomnia where a person engages in activities (usually walking) while in a state of partial arousal from deep non-REM sleep. Sleepwalking typically happens in the initial third of the night, as the body is in the deepest sleep stage.
A person who is sleepwalking may walk around the house, get out of bed, and even leave the house, all while being unaware of their actions.
During a sleepwalking episode, a sleepwalker's eyes may be open but with a blank or glazed expression, and they are usually unaware of any extraneous stimuli and hard to fully awaken. Upon awakening, a sleepwalker may be confused or disoriented and generally has no recollection of the sleepwalking incident.
Sleepwalking is most common in children between 4 and 12 years, but can continue through the ages or even begin later in life, often precipitated by stress or fatigue, medications, or medical conditions.
Symptoms of Sleepwalking
Following are the main symptoms of sleepwalking:
- Sitting up in bed while asleep
- Walking around with a blank or dazed expression
- Unresponsiveness to external stimuli or conversations
- Difficulty waking the person during an episode
- Performing routine activities while asleep
- Open eyes with a glassy or empty look
- Confusion or disorientation upon waking
- No memory of the event after waking
- Talking or mumbling during the episode
- Exhibiting unusual behaviors (e.g., urinating in inappropriate places)
Causes of Sleepwalking
A variety of physical, psychological, and genetic factors may lead to sleepwalking as they disrupt deep sleep. Understanding these risk factors may inform your ability to prevent and deal with sleepwalking episodes.
Sleep DeprivationWhen a person is too tired to be awake, they are likely to exhibit deeper stages of non-REM sleep known as sleep deprivation, which increases the chances of partial arousals and consequently sleepwalking.
Stress or AnxietyHigh emotional stress and anxiety that is present in our lives can disrupt our sleep, lead us to sleep restlessly, and can increase our chances of sleepwalking episodes.
Irregular Sleep PatternA sleep schedule that is constantly fluctuating can disrupt the circadian rhythm and disrupt the sequence of sleep stages, and this can lead to parasomnias such as sleepwalking.
Fever (especially in children)High body temperature associated with illness can lead to brain arousals during deep sleep, regardless of whether the child is conscious of the arousal, and therefore lead to sleepwalking.
Genetics PredispositionSleepwalking tends to run in families and has hereditary connection. If one or both parents experience sleepwalking episodes, their children have increased chances of experiencing episodes too.
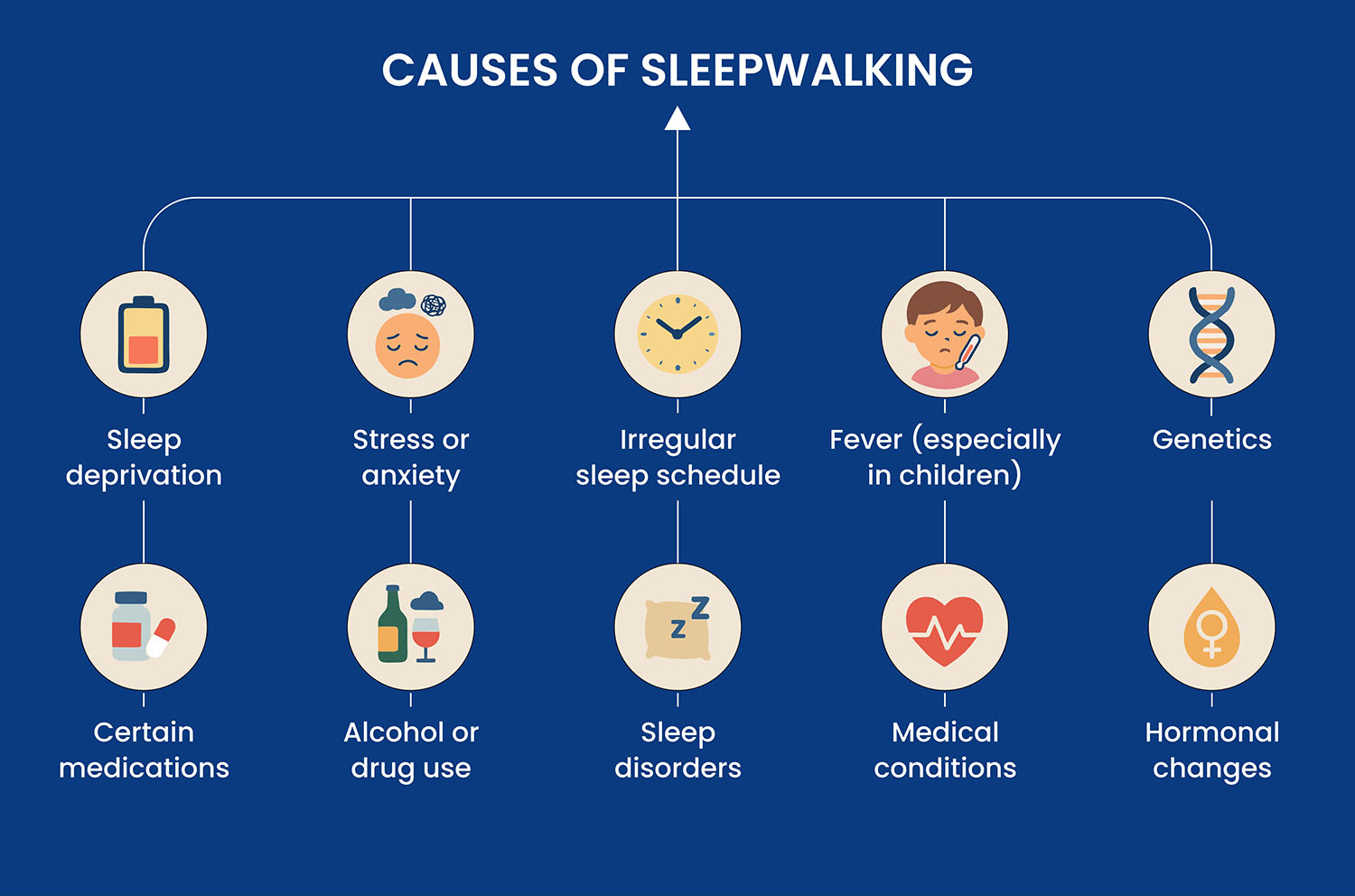
Drugs that have an effect on the central nervous system (CNS) such as sedatives, antihistamines, or some antidepressant medications may alter nerve processes while a person sleeps or in some cases trigger sleepwalking episodes.
Alcohol or Other SubstancesUsing alcohol or recreational drugs can interfere with the restorative nature of sleep, fragment sleep, and increase the chances of a partial awakening from deep sleep.
Sleep ProblemsConditions such as obstructive sleep apnea or restless legs syndrome can lead to repeated awakenings during the night, which can cause sleepwalking behavior.
Medical ConditionsSome other physical health conditions, such as gastroesophageal reflux disease (GERD) or nocturnal seizures, can disrupt deep sleep and provoke sleepwalking.
Hormonal ChangesPuberty, menstruation, or other hormonal changes may impact sleep and increase sleepwalking susceptibility, especially among teenagers.
Severe Risks of Sleepwalking
Falling from heights: A sleepwalker may not realize they are walking off of stairs, a balcony or a window.
Leaving the residence: Wandering outside introduces the person to dangers, exposure to extreme temperatures or weather conditions, or getting lost.
Driving while asleep: In rare circumstances, a person may seek to drive a vehicle while in an episode which could threaten life.
Using sharp, dangerous or potentially hazardous objects: The person may use tools, manipulate knives or cook while completely unaware.
Violent or aggressive behavior: Some people may unknowingly hurt themselves or someone else if they are entered to an episode and are surprised.
Chronic sleep deprivation: Leads to chronic fatigue, loss of attention, and an increased chance of poor mental health.
Risk to minor children or other members of the household: In severe cases, episodes may disrupt co -sleepers or may pose a danger to family members.
How to Diagnose Sleepwalking?
The diagnostic process for sleepwalking will usually involve a thorough medical history and sleep questionnaire, sometimes with the help of family members or bed partners who have witnessed sleepwalking episodes. The health care provider may inquire about sleep habits, levels of stress, medications being taken, and family history of sleep disorders.
Providers frequently ask whether a patient has been keeping a sleep diary with details of their sleep patterns or episodes, recording any possible triggers, and frequency. Providing a sleep diary for 1–2 weeks can help identify these patterns and triggers.
If the patient's condition is worse, or unclear, a polysomnography or sleep study may be arranged. A polysomnography is an overnight study that will record brain activity, heart rate, breathing, and movement to see if there are any abnormal sleep patterns or to rule out other medical conditions such as obstructive sleep apnea, or nocturnal seizures.
If warranted, the provider may recommend neurological or psychological assessments for underlying conditions contributing to the sleepwalking.
Sleepwalking Treatment
Treatment of sleepwalking centers on improving overall sleep quality and eliminating triggers, and also making the sleepwalking as safe as possible during occurrences. Overall, sleepwalking is not dangerous and most systems, especially in children, are benign and improve with age. However, if it is happening often, dangerous, or disruptive, more formal and structured treatment may be warranted.
1. Improving sleep hygiene
When trying to improve sleep hygiene, consistency in sleep times is going to be key. Going to sleep and waking at the same time every day (including weekends) helps with the sleep cycle.
Having a calming routine before bed (e.g., bath, music, no screens) that promotes restful, deep, and uninterrupted sleep, and limiting caffeine, heavy meals, and alcohol close to bedtime will help to improve sleep hygiene.
2. Stress and anxiety management
Emotional stress is a common trigger for sleepwalking with adults. Using techniques previously mentioned (deep breathing, progressive relaxation, meditation or yoga, etc.) can help lower emotions before bed.
In cases of chronic anxiety, trauma, or emotional triggers associated with sleepwalking, some type of therapy, such as Cognitive Behavioral Therapy (CBT), is possible treatment if warranted.
3. Safe sleep environment
It is important to create a sleep environment that is as safe as possible to avoid injury when sleepwalking:
- Lock doors and windows
- Remove sharp objects or tripping hazards
- Use bed alarms or motion detectors if needed
- Sleep on the first floor, especially for children or severe cases
4. Scheduled Awakenings
For habitual episodes that occur at predictable times, a method known as scheduled awakenings may be useful. This involves gently waking the person approximately 15–30 minutes before he typically sleeps walks in a night, and letting him return to sleep. This may reset the sleep cycle and reduce episodes.
5. Medication (in Severe Cases)
Medication should not be the first course of treatment in most cases; however, in circumstances where nothing else is effective, it can be prescribed. Options may include:
Benzodiazepines (e.g. clonazepam) – used to decrease the number of deep sleep arousals
Antidepressants – sometimes used if sleepwalking is related to underlying depression or anxiety.
Melatonin – used when sleepwalking is related to disruption in circadian rhythm Medication should only be used if prescribed by a healthcare provider (especially when children are involved).
6. Treating Underlying Conditions
If the sleepwalking is a result of or exacerbated by another condition - for example sleep apnea, GERD, or seizures, treating the causative issue is critical. If the underlying conditions are treated, episodes may significantly reduce or even disappear altogether.
7. Psychological Evaluation (if needed)
In more complicated situations, a psychological or neurological evaluation may be recommended to rule out possible mental health or neurological causative conditions. This is especially important for adults whose sleepwalking began suddenly, or include dangerous behavior.
Final Thoughts
The sleep disorder of sleepwalking or somnambulism can range from harmless to dangerous for both children and adults. Sleepwalking is triggered by stress, insomnia and/or medical conditions, although most cases improve with good sleep hygiene, reduced stress and a safe environment. If sleepwalking is severe or frequent, however, you might want to seek medical advice to help keep you safe and to best manage your sleepwalking episode.













