Post-Traumatic Stress Disorder (PTSD) affects millions of people around the globe. Approximately 1 in 13 people will experience PTSD at some point in their life! The National Center for PTSD estimates that in the U.S. there are about 12 million adults experiencing PTSD in a given year.
PTSD usually occurs after being exposed to very distressing experiences, and usually creates bad and lasting consequences. Most noticeably, it interferes with the normal ability to sleep, process emotions, socialize, and maintain relationships needed to function daily.
This blog will address some of the causes, symptoms, and evidence-based treatments to assist individuals and their families to regain control of their lives and move on.
What is Post Traumatic Stress Disorder?
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after someone encounters or experiences a traumatic episode, such as:
- military/war combat
- sexual assault
- natural disasters
- severe accidents
- violent assaults
- bullying
- verbal abuse
- loss of a loved one
PTSD is a reaction to prolonged experience of stress after the danger has passed, and the stress response continues, even at high levels, resulting in serious, troublesome thoughts, re-experiencing/flashbacks, emotional numbing, and avoidance of triggers.
PTSD can happen to anyone and doesn't discriminate by age or background. PTSD can be detrimental to daily living, relationships, or overall life satisfaction, if left unresolved with the proper supports or treatment plan.
Studies demonstrate that people with PTSD are more than twice as likely to also be suffering other co-occurring disorders, such as depression, anxiety, and substance abuse. While there is greater awareness of PTSD and progress in developing medications and psychotherapies to treat PTSD, early detection and treatment is critical to recovery and improvement in quality of life.
Types of PTSD
Acute PTSD
This type of PTSD occurred shortly after experiencing a traumatic event (or events). The duration of symptoms related to acute PTSD is generally less than three months. Most trauma survivors fully recover from acute PTSD, particularly when they receive appropriate care and timely interventions.
Chronic PTSD
PTSD is considered chronic when it lasts for longer than three months. Chronic PTSD can have a profound effect on day-to-day functioning and typically requires treatment or therapy for the long term.
Delayed-Onset PTSD
In this instance of PTSD, symptoms do not appear immediately after the trauma, instead, symptoms develop at least six months later, and in some cases years, after the traumatic event. New or unexpected circumstances can provide a trigger for the onset of delayed PTSD with clear connections to a prior trauma.
Complex PTSD (C-PTSD)
Complex PTSD (C-PTSD) arises from long-standing, repeated or prolonged trauma (such as childhood abuse, domestic violence or being held hostage/ captive). C-PTSD includes all the symptoms of PTSD and additional difficulties with emotional regulation, interpersonal relationships and issues with one's sense of self (feeling foggy, detached, etc.).
Comorbid PTSD
Comorbid PTSD occurs in the presence of one or more other mental health disorders (such as depression and anxiety disorders, or substance use disorders). Co-occurring conditions can make it more difficult to diagnose PTSD, and treatment often requires a holistic, comprehensive, and integrated approach to therapy.
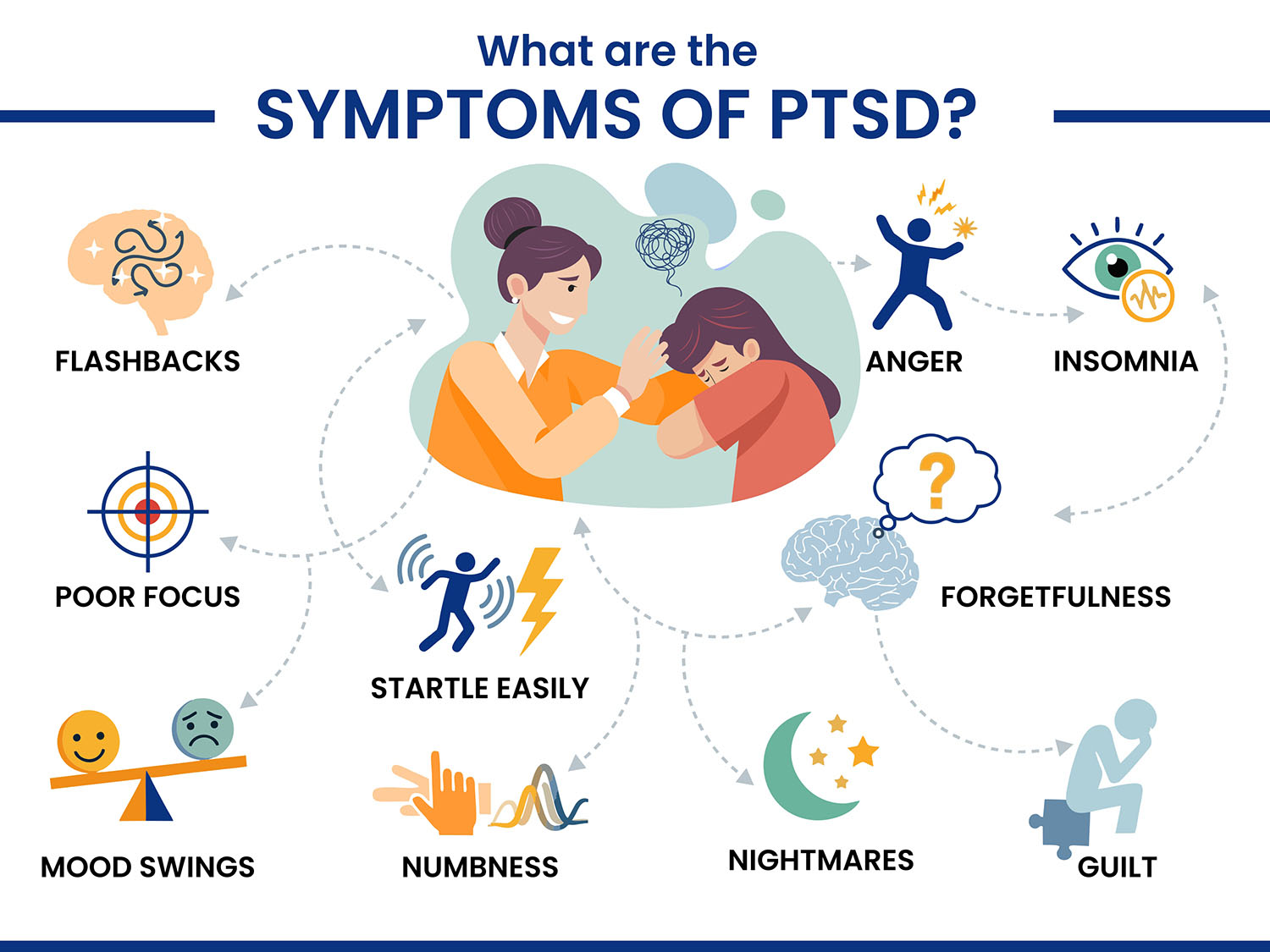
PTSD Symptoms
Post-Traumatic Stress Disorder (PTSD) symptoms can include:
- Intrusive memories or flashbacks of the trauma
- Nightmares or distressing dreams
- Increased emotional distress or physical reaction to cues of the trauma
- Avoidance of places, people or activities that remind the person of the trauma
- Negative shift in thoughts and mood (e.g., feeling hopeless, problems with memory, feeling release)
- Ongoing negative emotion (e.g., fear, guilt, anger, shame)
- Hyper-arousal (e.g., irritability, angry outbursts, startle response)
- Trouble sleeping or concentrating
- Feeling detached from others or a sense of no interest in things the person previously enjoyed
Symptoms of PTSD can vary in severity and can worsen when the individual is stressed or again exposed to trauma-cues.
How Common is PTSD?
Post-traumatic stress disorder (PTSD) is more prevalent than most people think. Global estimates show that 3.9% of the general population will develop PTSD during their lifetimes, which means that approximately 6 out of every 100 in the United States (6.8%) will develop PTSD in their lifetime.
The occurrence of PTSD is especially higher among subpopulations and groups, such as veterans, those who have been assaulted, victims of natural disasters, or extremely serious accidents. Signs of PTSD in women are twice as likely to develop PTSD than men.
Can Children Have PTSD?
Yes, children can develop post-traumatic stress disorder following a traumatic experience themselves or having witnessed a traumatic experience. Traumatic events may include physical or sexual abuse, accidents, natural disasters, serious illness, or an unexpected death of a parent or caregiver.
Children process trauma differently than adults and may exhibit symptoms in different ways, often showing symptoms through changes in behavior, mood, and development. The following are the PTSD symptoms in children:
- Re-experiencing the trauma – Nightmares, flashbacks, and distress when reminded of the event.
- Avoidance – Withdrawal from people, places, or activities that remind them of the traumatic event.
- Regression – Return to behavior like bed-wetting or thumb-sucking.
- Sleep disturbances – Difficulty falling and/or staying asleep; often frequent nightmares.
- Irritability or aggression – Angry outbursts, tantrums, or acting out behaviors in the home or at school.
- Anxiety or fearfulness – Persistent worry, fear of separation from parents, exaggerated startle response.
- Trouble concentrating – Difficulty concentrating in class or completing a task.
- Physical complaints – Headaches or stomachaches with no medical explanation.
- Low self-esteem – Perceived guilt, shame, or worthlessness related to the traumatic experience.
You can help children deal with their symptoms through early identification and trauma-informed treatment, like Cognitive Behavioral Therapy (CBT) for children.
PTSD Post Pregnancy (Postpartum PTSD)
Postpartum Post-Traumatic Stress Disorder is a psychiatric condition that can develop after a non-normal birth experience. While childbirth is typically viewed as a celebration, some women view it as an unhealthy physical and emotional experience.
Triggers for PTSD can include:
- emergency C-section,
- unwanted interventions,
- a sense of loss of control, and
- inadequate support from the medical team.
In extreme situations, triggers can be:
- stillbirth,
- injuries to the baby during birth, and
- significant complications, threatening the life of the mother or the infant.
Postpartum PTSD is different from postpartum depression, with PTSD involving trauma and fear, flashbacks and emotional numbness. PTSD is under recognized, and this can interfere with maternal-infant attachment and maternal mental health.
Women with previous trauma history, a history with anxiety or lack of emotional support, are at more risk. PTSD can also be exacerbated by changes in hormones, lack of sleep, and isolation after giving birth.
Common Symptoms of Postpartum PTSD
- Intrusive flashbacks or nightmares related to childbirth,
- Avoidance of reminders of the birth (e.g., hospital visits, talking about the birth)
- Emotional numbness or detachment from the baby or loved ones
- Hyperarousal, including irritability, difficulty sleeping, or being easily startled
- Difficulty bonding with the baby
- Feeling helpless, anxious, or on edge constantly
- Persistent negative mood or thoughts
Postpartum PTSD can result in long-lasting emotional concerns, disruption to family dynamics, and infant delays due to interrupted mother-infant bonding/interaction. Therefore, seeking help is critical.
Treatments such as trauma-focused Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization Reprocessing (EMDR), and support groups are often effective.
Early identification, and understanding by healthcare providers during childbirth and afterward will lessen potential the effect of postpartum PTSD and establish an opportunity for mothers to heal.
What Causes Post-traumatic stress disorder (PTSD)?
Post-Traumatic Stress Disorder (PTSD) occurs when the brain alters the way it reacts when experiencing or witnessing a traumatic event. If a person is exposed to extreme fear, shock, or helplessness, it can hyper-stimulate the natural stress response, which interferes with the way the brain organizes and stores memories, particularly when referencing the trauma.
The key brain structures in PTSD are:
- Amygdala: becomes hyperactive and elicits increased fear and emotional responses.
- Hippocampus: may shrink or be dysfunctional, impeding the ability to differentiate between danger in the past and any imminent danger in the present.
- Prefrontal cortex: becomes underactive, leading to an inability to self-regulate emotional responses or rationalize fears.
These changes create challenges for people with PTSD. Flashbacks, nightmares, hyper vigilances, avoidance, and other symptoms occur because individuals with PTSD keep their nervous systems in a persistent state of “fight or flight;” even when a safe environment surrounds them. Prolonged elevated arousal can interfere with a person's ability to function and maintain emotional balance.
Risk Factors of PTSD
You cannot predict who will develop PTSD after experiencing a trauma. PTSD tends to occur more frequently in individuals who have:
- Experienced or witnessed severe trauma (i.e., violence, assault, war, disaster)
- A personal history of mental health disorders (i.e., anxiety, depression, etc.)
- Childhood abuse or neglect
- Little to no support system
- A previous history of trauma
- A history of substance abuse
- Experiences involving a high level of stress (i.e., military deployment, emergency services)
- A family history of anxiety or mood disorders
- Prolonged or repeated trauma
- Are women (higher incidences reported in females)
- Someone with a particularly intense or sudden traumatic experience (i.e., sudden death of a loved one)
How Does PTSD Affect Sleep?
PTSD can have a substantial impact on sleep, as it keeps the brain and body in a state of hypervigilance. After a traumatic experience, the brain’s fear response system (especially the amygdala) may remain in overdrive which means a person with PTSD may feel as if they’re constantly under threat or in danger, even when in a safe situation, thus making it impossible to relax and fall asleep.
Some individuals with PTSD might experience repetitive nightmares about the trauma, which are often followed up by jolting awake and fearing trying to go back to sleep, a.k.a. Sleep anxiety. Some individuals have night terrors or flashbacks while asleep, creating fears of sleep altogether. The chronic lack of sleep can lead to insomnia, where they cannot fall asleep, or wake several times through the night.
The hyperarousal component, one of the major hallmark symptoms of having PTSD, is another important factor. This means a person with PTSD is always "on edge” and on the lookout for danger. This constant state of hypervigilance inhibits their body's ability to enter the deeper, restorative stages of sleep.
Over time, if poor sleep persists then other PTSD symptoms like irritability, distractibility, and emotional stability can worsen and create a vicious cycle where your insufficient sleep exacerbates your PTSD, and it in turns continues to impact your sleep.
The appropriate treatment for PTSD, including therapy, and sometimes medication, can help manage the sleep issues that may be a consequence of your trauma.
PTSD Diagnosis
The diagnosis of Post-Traumatic Stress Disorder (PTSD) typically involves clinical assessment, mental health assessments, and then consideration of DSM-5 criteria. And generally, a healthcare professional will almost always be a psychiatrist or psychologist as they will require a thorough psychological evaluation that will include a discussion of the patient's symptoms and trauma history, emotional health, and functioning in daily life.
Generally, A person receiving a diagnosis of PTSD needs to have experienced or witnessed a traumatic event and have a range of different symptoms - such as:
- intrusive memories
- avoidance
- negative alterations in thinking and mood, and
- hyperarousal - for at least one month.
They often use standardized questionnaires (e.g., PTSD Checklist (PCL-5)) and screening tools to document and screen for PTSD severity and symptoms. Sometimes, they will run physical exams as well to assess, just to eliminate if it is not another health issue with mimickers of PTSD. Getting diagnosed as early as possible and accurately is of utmost importance for success in treatment and recovery.
PTSD Treatment
PTSD is typically treated with a combination of therapies, medication, and other support-based approaches. Individual treatment is based on the severity of symptoms and history. PTSD treatment generally follows this outline:
1. Psychotherapy
Cognitive Behavioral Therapy (CBT): Assists individuals in identifying, understanding and changing their negative thinking and behavior patterns related to trauma.
Prolonged Exposure Therapy (PE): A patient recalls trauma memory and feels associated feelings gradually and confronted situations to alleviate fear.
Eye Movement Desensitization and Reprocessing (EMDR): A health care professional helps the patient process their traumatic memories by following their finger with their eyes.
Cognitive Processing Therapy (CPT): A patient challenges their unhelpful beliefs about the trauma and modifies them.
2. Medications
Antidepressants: SSRIs such as paroxetine and sertraline are FDA-approved for use in treating PTSD symptoms.
Antianxiety medications: Should only be used on a limited basis to treat severe anxiety or panic attacks.
Prazosin: Commonly prescribed to help reduce nightmares and improve sleep.
Mood stabilizers or antipsychotics: May be prescribed for extreme mood swings or co-occurring disorders.
3. Supportive Methods
Group therapy: can give clients the benefit of shared experiences as well as emotional support from others with PTSD.
Family therapy: allows families to better understand the disorder and help support recovery.
Self-care and healthy lifestyle changes: Regular sleep, exercise, mindfulness, and reduced alcohol or substance use.
Can You Prevent PTSD?
Post-Traumatic Stress Disorder (PTSD) cannot ultimately be completely prevented, especially if the trauma was sudden or very intense. However, getting timely emotional support, and early intervention can decrease the risk of having more complicated or severe PTSD symptoms.
It is possible to decrease the risk of developing PTSD, and although no strategy is guaranteed to prevent PTSD, the following precautions can substantially reduce the risk.
Tips to reduce the risk of developing PTSD:
- Immediately after a traumatic event, seek professional support to help process your emotions.
- Stay connected with trusted friends, family, or support groups to remain connected to others and counter any tendencies towards social isolation.
- Utilize stress management techniques like mindfulness, meditation, and deep breathing exercises.
- Do not use alcohol or drugs to cope after your traumatic experience.
- Get adequate sleep on a regular basis and prioritize rest to facilitate emotional healing.
- Consider short-term counseling and or trauma-informed therapy if needed to work through some of your distress right after getting traumatized.
- Build emotional resiliency with healthy habits of living and healthy coping strategies.
- Be mindful of your mental health/diagnosis history - for individuals with past trauma histories or anxiety diagnoses, usually, access to early preventative services is a good option for them.
Final Thoughts
PTSD is a prominent mental health disorder and is treatable. PTSD can affect anyone who has experienced trauma, but acknowledging early signs, seeking prompt help, and exploring avenues of treatment may be all that is needed in that situation. With proper support, people can gain control of their lives and enhance their emotional health.













