By 2030, more than 1.2 billion women will be in menopause or post-menopause. And one of the most common symptoms reported during this time is disrupted sleep. Research shows that 30-60% of women can experience insomnia, night sweats, staying asleep, or waking up frequently during the night during the menopausal transition. While hormonal fluctuations create changes in the body, they also alter our brain's cycling through sleep.
This blog describes stages through which women navigate the menopausal transition, the real impact on quality of sleep, and the proven sleep tips to help women obtain better sleep in menopause.
Understanding the Process of Menopause
Menopause is the biological stage that occurs when a woman has permanently stopped having menstrual periods. This happens because the ovaries stop releasing eggs, and the production of hormones (especially estrogen + progesterone) declines substantially.
Menopause can be officially confirmed when a woman has not had menstrual periods for 12 consecutive months (not due to pregnancy, medication, or illness).
Menopause naturally occurs between the ages of 45–55 years (the average age is around 51). It can also occur early due to surgical removal of the ovaries, certain medical treatment (such as chemo), or certain health conditions.
Menopause is not a single point - rather a transition process which includes:
-Perimenopause- the years before menopause when symptoms begin.
-Menopause - 12 months without a period.
-Postmenopause - after the menopausal state is established.
This transition may influence sleep, temperature regulation (hot flashes), emotional regulation, weight, heart health, metabolic functioning, bone density, and overall energy.
Stages of Menopause
1. Perimenopause
This is the transition period where estrogens and progesterone begin fluctuating - sometimes high, sometimes low - which triggers symptoms. The period may still come, but may become irregular.
This is the phase when most women start to notice changes, like hot flashes, fluctuations in mood similar to their PMS phase, disruption of sleep, night sweats, surges of anxiety, and periods that become heavier or lighter.
This phase may last anywhere from a couple of years up to nearly 10 years.
2. Menopause
This is the recognized point of time that is 12 months without a period-meaning naturally, not due to a birth control, surgical procedure, or medication. Ovulation has ended. Estrogen is low, and fertility has officially ceased.
3. Postmenopause
This time frame is every year following menopause. Symptoms can persist for a while-for some get milder, for others worse, before it moderates. Health effects and risks also change during this time frame-bone loss accelerates, metabolism is more easily influenced, and more sensitive to low estrogen in blood vessel and heart health.
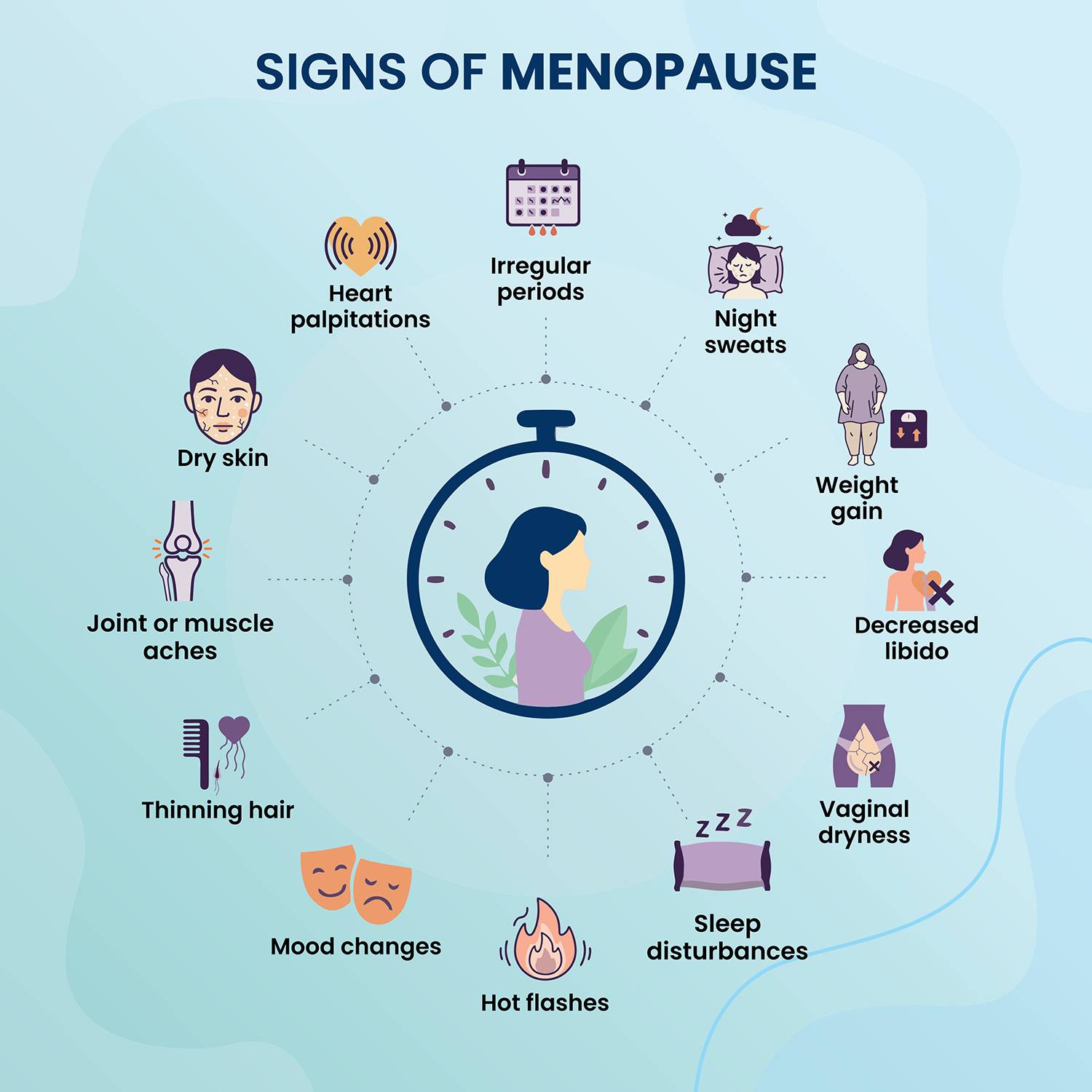
Signs of Menopause
1. Perimenopause
Women typically report the following symptoms and signs during the menopause transition:
- Unexpected or absent menstrual cycles
- Hot flashes
- Night sweats
- Sleep difficulties or sleep interruptions
- Sudden changes in mood
- Increased feelings of anxiety or irritability
- Fatigue and low energy levels during the day
- Brain fog or difficulty focusing or concentrating
- Vaginal dryness
- Increased occurrence of headaches
- Lower levels of libido or changes in sexual arousal
- Weight gain, particularly around the abdomen
- Loss of muscle or changes in body composition
- Joint discomfort, pain, or ache
- Dryer skin or thinning hair
These signs do not usually emerge at once, but accumulate gradually over time during the perimenopause and reach their maximum wad of symptoms at menopause, before continuing on into the postmenopause in varying degrees of severity.
How Does Menopause Impact Your Sleep?
Sleep is impacted by menopause directly due to changes in the hormones that previously stabilized sleep, temperature, and calmness: estrogen and progesterone.
Once these hormones drop and begin to fluctuate, it temporarily disrupts several systems.
Here’s what actually happens:
1. Night temperature shifts create instability in sleep
They spike body temperature, which disturbs sleep. When the body overheats, it wakes you often, and your sheets are soaked, making it difficult for the brain to sustain deep stages of sleep to feel fully rested.
2. Decreased levels of progesterone impact relaxation
Progesterone naturally has a calming, sleep-inducing effect. When it lowers, women lose that natural sedative-like support that assists in their fall asleep routine.
3. Drop in estrogen affects serotonin and melatonin production
These hormones play a significant role in sleep. When estrogen drops, serotonin decreases → mood feels off balance. Melatonin decreases → circadian rhythm is disrupted. Result: lighter sleep, waking more often, and harder to fall asleep again.
4. Anxiety + hypersensitivity occur
Many women notice a racing mind, intrusive thoughts, and/or a sudden increase in worry as they are getting into bed. This is not what you would call “personal stress” — this is brain chemistry that is affected by hormones.
5. Increased risk for sleep-disordered breathing
Postmenopausal women are also at a higher risk for snoring or sleep apnea, both due to airway tissues changing as a result of a decrease in hormones.
Sleep-disordered breathing is a well-known hidden contributor to chronic insomnia in midlife women.
6. Increased sensitivity to pain and joint discomfort
Falling estrogen also increases inflammation and joint stiffness, and when the body is uncomfortable, it is more difficult for the mind and body to settle into and stay asleep.
Sleep Aids for Good Sleep During Menopausal Years
Here are some helpful sleep aids for improved sleep during menopause—along with helpful information about the aids, how they work, and things to check. (You should always check with your doctor before starting any new form of approach.)
Non-pharmacological strategies (first-line)
-Cognitive Behavioural Therapy for Insomnia (CBT‑I): Tailored for thoughts and behaviours around sleep, CBT-I is more effective than sleep hygiene education for insomnia during menopause.
-Sleep hygiene & environment: A consistent sleep schedule, a cool and dark room, limiting screen time before bed, and avoiding heavy caffeinated drinks and alcohol late in the day – all support hormonal transitions and optimize the sleep system in midlife.
-Managing vasomotor symptoms (hot flashes/night sweats): They are a strong influence on awakenings. One review indicated that the prevalence of nighttime awakenings is higher during menopausal transition.
Nutritional, supplement & herbal aids
-Melatonin: Melatonin also helps to regulate the cycle of sleep and wakefulness, which is often disrupted with lower estrogen/progesterone. Studies in menopausal women have demonstrated melatonin benefits, but evidence is more variable.
-Holistic and herbal options: Herbal extracts such as Lemon balm + Valerian root have shown some modest sleep benefit in menopausal women (e.g., one study noted that 20-36% of participants slept better with lemon balm + valerian root tea.)
-Foods/drinks that promote relaxation: Drinking warm milk, chamomile tea, or tart cherry juice - these foods and/or drinks are not a miracle cure for sleep problems, but they have very low risk and may help in the wind-down process.
-Other nutritional interventions: More studies are showing that various types of nutritional/supplement interventions may show beneficial effects for sleep in post-menopausal women than not. However, the quality of the evidence is variable.
Hormonal & pharmacological treatments (under medical guidance)
-Hormone therapy (HT or MHT): This may provide some relief when sleep symptoms are strongly associated with vasomotor symptoms. However, hormonal treatment is not a primary indication for insomnia alone, and must involve a risk/benefit tradeoff on a case-by-case basis.
-Sleep medications: In some instances, hypnotics or sleep-specific medications may be utilized, although results in menopausal women are mixed, and this population also has to consider side effects.
When to See a Doctor?
You may want to consider getting medical assistance if:
- Sleep issues are occurring 3 or more nights a week for several weeks.
- Night sweats, or hot flashes, are severe enough to routinely disrupt sleep.
- You awaken gasping, choking, or snoring (potentially with sleep apnea).
- You have gone through the typical sleep hygiene and/or supplement improvements to no avail.
- Notable mood swings, anxiety, and/or depression are experienced with sleep issues.
- You have unexplained weight gain, chronic fatigue, or sudden body pains.
- You suspect you might be experiencing early menopause (before age 45).
- You are experiencing irregular bleeding after menopause (red flag).
A healthcare provider can evaluate hormonal levels and determine other sleep disorder options that are underlying for safe treatment options, including hormone therapy, medications, or targeted sleep therapies that are targeted.
Final Thoughts
Difficulty sleeping during menopause is not your fault; it is due to changes produced by the hormones. The positive note? Sleeping can be better. From cooling the sleep space down to modifying your routines, to targeted supplements or guidance from a physician, there are many effective options. In the right conditions and with the right help, you can experience restful nights again during menopause and after menopause.













